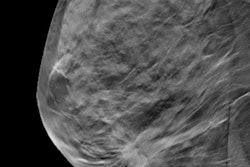
A new study published March 15 in JAMA Internal Medicine claims that breast cancer centers are promoting mammography screening for women in their 40s, contrary to guidelines from the U.S. Preventive Services Task Force (USPSTF). Imaging experts are disputing the findings.
Researchers analyzed websites of 606 U.S. breast cancer centers and found that of those that recommended an age at which to start screening, 87.2% recommended that women begin at age 40, which the authors maintained contradicts guidance from national societies. And of those that provided a screening age as well as a screening interval, 80.9% recommended annual screening starting at the age of 40.
In contrast, the USPSTF guidelines for screening mammography, last updated in 2016, advise screening every two years between the ages of 50 and 74 and that screening for women in their 40s should be based on an individual evaluation of risks and benefits. The American Cancer Society (ACS) recommends annual screening for women between the ages of 45 and 55.
"The public advice provided by high-volume breast centers in the [U.S.] suggests that these centers may prioritize factors not reflected in the data, such as patient and physician preferences, recommendations from specialty (e.g., radiology) societies, concerns about litigation, or possible financial considerations," wrote a team led by senior author Dr. Jennifer Marti, assistant professor of surgery at Weill Cornell Medicine, and colleagues.
Marti et al conducted the study to investigate a hypothesis that many specialized breast centers in the U.S. are not offering information on screening mammography in line with guidelines from national medical societies.
"The American Cancer Society and USPSTF recommendations reflect data indicating the potential harms of earlier screening, which include false-positive findings, unnecessary biopsies and operations, anxiety and discomfort, overdiagnosis and overtreatment of indolent cancers, and costs of low-value care," the authors explained.
Out of 606 breast centers considered in the study, 487 (80.4%) provided recommendations for screening on their websites. And of these, 429 (88.1%) recommended a starting age and a screening interval.
| Screening recommendations from U.S. breast cancer centers | |
| Starting age | Percent recommending |
| 40 | 77.2% |
| 45 | 7.2% |
| 50 | 4.1% |
| Discuss with physician | 11.5% |
| Screening interval | Percent recommending |
| Annual | 72.7% |
| Annual or biennial | 12.1% |
| Biennial | 3.3% |
| Discuss with physician | 11.9% |
Primary care/specialist divide
Recommending annual mammography in women younger than 50 years is confusing and likely to conflict with advice from primary care physicians, wrote University of California, San Francisco cardiologist Dr. Rita Redberg and colleagues in an editorial also published March 15 in JAMA Internal Medicine. Redberg is also editor in chief of the journal and is a frequent critic of screening exams, including both breast and lung screening.
"Breast cancer centers with clear financial benefits from increased mammography rates may wish to reconsider offering recommendations that create greater referral volume but conflict with unbiased evidence-based USPSTF guidelines and have the potential to increase harms among women," the authors advised.
In a joint statement, the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) said that breast centers are following national guidelines. The ACR, the SBI, and the American Society of Breast Surgeons recommend annual mammograms starting at age 40 and the American College of Obstetricians and Gynecologists recommends screening starting at age 40 every one to two years. The statement also noted that Black women are more likely to get breast cancer early and to die from the disease.
The results of the new study are not surprising; rather they confirm that breast cancer experts in the U.S. have looked deep into the data and do not support the USPSTF screening guidelines and do not recommend them for their patients, said Dr. Dana Smetherman, who chairs the ACR's commission on breast imaging.
Currently, there is a moratorium delaying the use of USPSTF's latest recommendations, so there is not an impact on reimbursement for more frequent screening.
"The USPSTF has a lot of power," Smetherman, chair of radiology at Ochsner Health, told AuntMinnie.com. "If you think about underserved communities -- those most at risk -- they almost certainly couldn't pay for these examinations."
Smetherman also said she is extremely concerned about the suggestion of a financial motivation on the part of breast centers, even though the study authors acknowledged that there was no evidence for this claim.
The data -- including randomized controlled trials, population studies, and modeling studies -- are clear that screening saves lives, but the question has been at what cost, commented Dr. Jessica Leung, president of the SBI. However, the ACR/SBI statement notes that the rate of over-diagnosis is actually only 2%.
Surveys have shown that women accept the risk for false positives and want to be screened, Leung, who is chair of breast imaging at the University of Texas MD Anderson Cancer Center in Houston, told AuntMinnie.com during an interview.
"We believe that 'costs' such as anxiety and overdiagnosis are greatly exaggerated and not valid," Leung said.