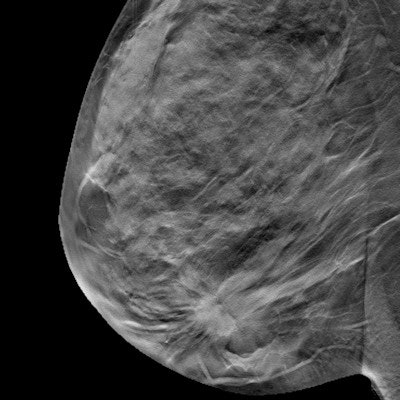
Medical media coverage emphasizes the benefits of 3D mammography screening while downplaying harms and ignoring conflicts of interest, according to new research published April 5 in JAMA Internal Medicine.
The findings further fuel the ongoing debate about the pros and cons of mammography screening -- and highlight a need for more objective reporting, wrote a group led by Mary O'Keefe, PhD, of the University of Sydney in Australia.
"Strategies to improve media reporting so that professionals, patients, and the public receive more balanced information about early detection tests are urgently needed," the team wrote.
Media attention to screening tests, particularly mammography, tend to be biased toward optimism, which can lead to what some consider harms, such as overdiagnosis, according to O'Keefe and colleagues.
"Higher quality reporting by journalists could encourage more healthy skepticism toward health options and curb overdiagnosis," the authors wrote.
To explore the level of bias in media reporting on screening tests, O'Keefe and colleagues evaluated 1,173 news stories covering benefits and harms associated with five different kinds of early-detection tests for asymptomatic patients, 579 of which covered 3D mammography for breast cancer. Stories included in the study came from a variety of news outlets, including newspapers, blogs, broadcast media, podcasts, and web news.
They found that among all the coverage, harms were mentioned but deemphasized in 27% (317 of 1,173 stories), and that overdiagnosis was mentioned in only 13% of the stories that mentioned harms (57 of 432). Overall, 63% of media coverage reported exclusively on the benefits of such testing.
There are real risks associated with routine mammography screening, especially for women between the ages of 40 and 49, wrote Tiffany Doherty, PhD, and Dr. Aaron Carroll from the Indiana University School of Medicine in Indianapolis in an accompanying editorial. The two noted that the U.S. Preventive Services Task Force (USPSTF) does not recommend routine screening in this age group.
"The harms include false-positive results, unnecessary biopsies and overdiagnosis and treatment of breast cancer that would not have become a health threat if left undetected," they wrote.
Yet, this isn't to say that mammograms are not important in breast cancer detection, according to Doherty and Carroll.
"They absolutely are [important]," they wrote. "But they have downsides as well as upsides, and we do not serve patients and the public well by focusing only on the latter or overstating the former."
In response to the study, Dr. Dana Smetherman, chair for the Commission on Breast Imaging for the American College of Radiology, said it makes "misleading assertions and outright false statements."
"It is disappointing that misinformation such as what is published in this article and invited commentary continue to confuse the public and risk the lives of women who deserve to have access to life-saving technology," Smetherman told AuntMinnie.com.
Multiple organizations agree that annual screening starting at age 40 saves lives, she said.
"Mammography has been shown to reduce breast cancer mortality in multiple studies and randomized control trials, as well as other modeling studies," Smetherman said.




















