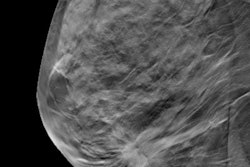
Recent advances such as digital mammography and tomosynthesis have not markedly improved the performance of mammography surveillance in women with a personal history of breast cancer, according to research published May 18 in Radiology.
Interval cancer rates, in particular, have not declined following the transition from film-screen mammography to digital mammography and remained substantially higher than those in the screening population overall, according to a team led by Dr. Janie Lee from the University of Washington.
"Because guidelines recommend mammography as the main breast surveillance imaging modality for women with treated breast cancer, our findings are relevant to current clinical practice, highlighting that technological advances over the last decade may not have improved surveillance outcomes," the group wrote.
Digital mammography and later digital breast tomosynthesis (DBT) have been replacing film-screen mammography over the last several decades. However, it has not been established if these technological advances have significantly improved diagnostic performance.
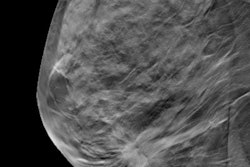
The researchers analyzed outcomes of surveillance mammography performed with digital mammography and DBT from 2007 to 2016 in women with a personal history of breast cancer. They then compared this to a 2011 study by Houssami et al, which was based on data collected from 1996 to 2007 in which mostly film-based mammography was performed. Benchmarks used to assess performance included interval cancer rate and cancer detection rate.
Among 32,331 women who underwent 117,971 surveillance mammographic exams (112,269 digital mammography and 5,702 DBT), the mean age at initial diagnosis was 59 years. Of these exams, 86,624 had a screening indication; for the rest, exams were performed either for a breast problem (19,638) or for short-interval follow-up (11,709).
| Performance of surveillance mammography with digital mammography and DBT | ||
| Film-screen mammography (Houssami et al) | Digital mammography + DBT | |
| Cancer detection rate per 1,000 | 6.8 | 8.5 |
| Interval cancer rate per 1,000 | 3.6 | 3.6 |
| Sensitivity -- overall | 65.4% | 70.4% |
| Sensitivity -- invasive second cancer | 61.1% | 66.0% |
| Sensitivity -- DCIS | 78.7% | 83.6% |
| Specificity | 98.3% | 98.1% |
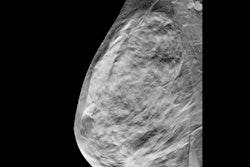
Of 1,418 second breast cancers diagnosed, 998 were surveillance-detected cancers and 420 were interval cancers. Researchers noted the interval cancers had characteristics that were associated with a poorer prognosis.
"Compared with previously published studies, interval cancer rate was comparable with rates from 1996 to 2007 in women with a personal history of breast cancer and was higher than the published digital mammography screening benchmarks," the researchers wrote.
Why didn't digital mammography and DBT show an improvement over analog technology? It's possible that the lack of a difference was due to the inherent similarities in mammography, regardless of whether its analog or digital, Lee wrote in an email to AuntMinnie.com.
"Digital breast tomosynthesis (DBT) is a technological advance that is still based in digital mammography. Improvements in cancer detection are likely related to being able to focus on a plane of tissue in a breast; removing tissue above and below that might obscure a cancer," Lee wrote. "DBT can also reduce 'false-alarms' from overlapping tissue that mimics a breast cancer. However, some limitations of digital mammography may still persist with DBT technology."
In an accompanying editorial, Dr. Linda Moy and Dr. Yiming Gao from New York University wrote that the study highlighted limitations of mammography inherent to methods.
"These data underscored the need to further understand how to improve surveillance practice in this heterogeneous population across disease and risk spectrum," they noted. "Current understanding of this important topic remains limited, and further investigations are warranted."
Lee and colleagues also said that more studies are needed to better determine the performance level of DBT for surveillance, as well as to identify women with a personal history of breast cancer who may benefit from adding supplemental imaging to their surveillance regimens.