Contrast-enhanced spectral mammography (CESM) is superior to conventional mammography and breast ultrasound when it comes to predicting underestimated ductal carcinoma in situ (DCIS), according to research published October 9 in Clinical Breast Cancer.
A team led by Dr. Hee Jung Shin from the University of Ulsan in South Korea also found that CESM is comparable to breast MRI in this area.
"CESM is a promising modality that shows the potential to assess both morphologies, including microcalcifications and perfusion characteristics, at lower cost and faster acquisition," Shin and colleagues wrote.
Wider acceptance of screening mammography is also increasing the rate of DCIS detection, with researchers saying DCIS accounts for 20% of screen-detected breast cancers. However, they also said that between 18% and 39% of DCIS at core-needle biopsy are initially underestimated and are later recategorized as invasive cancers after definitive surgery.
While it's rare that DCIS leads to nodal metastases, it may open the door for unnecessary biopsy, adding cost and inconvenience to patients.
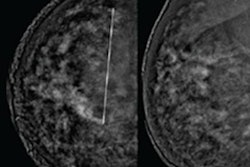
CESM has shown promise in recent years, with researchers highlighting that images can be obtained within the same session of breast positioning. This allows for direct comparison of enhanced locations on the contrast-enhanced recombined images to the microcalcifications on mammographic images.
Shin et al wanted to compare CESM with conventional mammography, breast ultrasound, and MRI when it comes to visualizing the extent of disease in patients with DCIS. They developed prediction models that utilized the four imaging methods.
They looked at data from 108 patients. A total of 113 lesions were analyzed, 50 being pure DCIS and 63 being underestimated DCIS.
| CEMS vs. other modalities for visualizing underestimated DCIS | ||||
| Mammography | Breast ultrasound | Breast MRI | CESM | |
| Pure DCIS | 44% | 76% | 80% | 58% |
| Underestimated DCIS | 73% | 81% | 92% | 86% |
Detection rates for both pure and underestimated DCIS were found to be significantly different for mammography and CESM, but not for breast ultrasound and MRI.
Additionally, no significant difference was found in the ability to predict DCIS underestimation based on models that included disease extent on breast MRI or CESM.
Underestimated DCIS was more likely to present as calcified lesions on mammography and enhancing lesions on CESM. Fibroglandular tissue density on mammography and background parenchymal enhancement on CESM and breast MRI were not found to be significantly different between pure and underestimated DCIS.
Underestimated DCIS was also associated with higher nuclear grade (p = 0.001), the presence of comedonecrosis (p = 0.026), and suspected invasion (p = 0.004) on preoperative core biopsy.
The researchers said their preoperative prediction model may be useful for surgeons who want to estimate the benefit of performing upfront sentinel lymph node biopsy.
"A further study comparing CESM and breast MRI in the prediction of DCIS underestimation in a larger population would be useful in validating our prediction model," the study authors wrote.