Artificial intelligence (AI)-based analysis of screening mammography exams could enable personalized cardiovascular risk assessment for women, according to a talk at the Society of Breast Imaging/American College of Radiology symposium.
Researchers from the University of Southern California and the Baker Heart and Diabetes Institute in Melbourne, Australia, evaluated the performance of a commercial AI software application for mammography that finds and quantifies breast arterial calcification (BAC) -- an underreported risk factor for cardiovascular disease.
Not only did the software correlate well with human readers, but it also identified additional cases that the readers missed.
"This automated software with quantification is a promising tool in enhancing communication of personalized cardiovascular risk in the female population, without additional radiation or exam time," said presenter Dr. Alyssa Watanabe of the University of Southern California.
Cardiovascular disease is the number one cause of death in women worldwide, but current risk prediction tools significantly underestimate risk, according to Watanabe. Female-specific risk markers are lacking.
Breast arterial calcification is identifiable on screening mammography but not routinely reported as it's not associated with malignancy. However, several observational studies have found a 2.5-fold increase in cardiovascular disease prevalence when breast arterial calcification is present, she said.
In their study, the researchers sought to compare human visual assessment of breast arterial calcification with AI-based software and to then assess the presence of cardiovascular disease and cardiac events in cases that had discordant evaluations. The research included a set of 2D screening full-field digital mammography exams from 285 women in the Monash Heart Database during 2016-2019. All patients had complete medical record data available for a cardiovascular workup within one year of the mammogram, according to Watanabe.
Of the women in the study, 48% had cardiovascular disease. Imaging -- coronary CT angiography, calcium score, coronary angiography, or functional imaging -- was used to make a diagnosis of cardiovascular disease in 104 women.
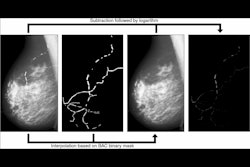
The mammograms were first reviewed by two fellowship-trained imaging readers, with discrepancies adjudicated by a third observer. The studies were then analyzed by cmAngio, an AI-based software application developed by AI firm CureMetrix. Watanabe is chief medical officer at CureMetrix, and first author Dr. Nitesh Nerlekar, PhD, of Baker Heart and Diabetes Institute serves as a clinical advisor to the company.
The software provides what it calls a Bradley score on a range of 0-100 based on features such as the breast arterial calcification area, extent, and intensity. A Bradley score higher than 5 is considered to indicate the presence of BAC.
The human readers detected the prevalence of breast arterial calcification in 30% of the exams, compared with 38% on the software. As for inter-reader agreement, the human readers had a kappa = 0.78. They also had high agreement with the software (r = 0.84).
| High performance for AI in detecting breast arterial calcification on digital mammograms | |
| Area under the curve (AUC) | 0.98 |
| Sensitivity | 94% |
| Specificity | 96% |
In other results, 23 cases with breast arterial calcification were missed by the human readers but spotted by the software. The missed cases had a median Bradley score of 7.5 (range, 5.25-16.95). Of these, 38% had cardiovascular disease and 9% had a myocardial infarction within the year of the mammogram, according to the researchers.
Larger prospective studies are now underway to further assess the performance of the software.
Disclosure notice: Dr. Alyssa Watanabe is chief medical officer of CureMetrix. Dr. Nitesh Nerlekar, PhD, serves as a clinical advisor to the company.