CHICAGO - Integrating digital breast tomosynthesis (DBT) into artificial intelligence (AI) shows superior performance to AI-mammography models, a study presented December 1 at the RSNA annual meeting showed.
In her talk, Su-A Yang from Lunit, Seoul, discussed results from the Lunit team's study that compared AI models using DBT and digital mammography. The researchers found that the AI-DBT model had higher area under the curve (AUC) and sensitivity in both fatty and dense breasts, as well as better performance for mass or asymmetry.
"We believe that a method to aid radiologists in reading DBT may be helpful in utilizing the full potential benefits of DBT," Yang said.
AI and DBT have entered the breast imaging landscape in recent years, with studies suggesting that AI is clinically useful in breast cancer screening alongside radiologists as another imaging reader. Other studies evaluating DBT meanwhile suggest that the modality improves cancer detection for fatty and dense breasts, the latter of which conventional mammography struggles with. However, DBT also has variable recall rates across radiologists in regard to experience, Yang noted.
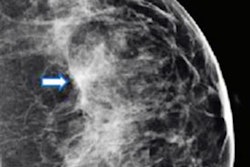
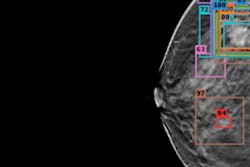
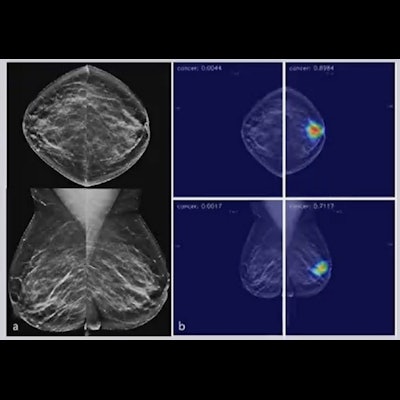
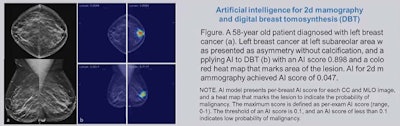 Research led by a team from Lunit showed that AI models using digital breast tomosynthesis perform better than models using digital mammography. Image courtesy of Su-A Yang.
Research led by a team from Lunit showed that AI models using digital breast tomosynthesis perform better than models using digital mammography. Image courtesy of Su-A Yang.The researchers wanted to compare the standalone performance of AI systems in DBT versus digital mammography. They looked at performance metrics related to breast density and mammographic findings. The team also wanted to see if AI for DBT could add to 3D information from DBT images.
The team looked at data from a total of 1,000 paired DBT and mammography examinations. They found that AI-DBT demonstrated superiority to AI-mammography in multiple areas.
| Comparison between AI-DBT, AI-mammography in overall breast cancer detection | |||
| AI-mammography | AI-DBT | p-value | |
| AUC | 0.852 | 0.925 | < 0.001 |
| Sensitivity | 78% | 91.2% | < 0.001 |
| Specificity | 76.9% | 74.9% | 0.306 |
For fatty and dense breasts, AI-DBT again showed significantly higher AUC and sensitivity than AI-mammography. This included AUCs of 0.933 (fatty) and 0.917 (dense) for AI-DBT, as well as sensitivity measures of 89.9% (fatty) and 91% (dense). As with the overall results, specificity between the two methods was comparable.
The researchers also found that AI-DBT increased the performance for mass or asymmetry without calcifications. AI-DBT had an AUC of 0.901 while AI-mammography had an AUC of 0.825 (p = 0.026).
Additionally, when it came to calcifications only, both AI methods had comparable performance (p = 0.75).
Yang said based on these results, AI-DBT could improve the feasibility of an AI system in breast cancer detection with higher diagnostic performance.