Rates of low-dose CT (LDCT) screening for lung cancer dropped significantly in the early months of the COVID-19 pandemic and haven't yet returned to expected levels, according to a study published February 3 in JAMA Network Open.
The trend was also seen in mammography breast cancer screening, wrote a team led by Christopher Doan of the University of Texas in Galveston. And although cancer screening rates appear to have recovered overall, the recovery is inconsistent and remains a concern.
"Interference with cancer screening by periodic surges in COVID-19 infections is a continuing problem," Doan and colleagues noted.
In the COVID-19 pandemic's early days, cancer screening rates decreased, which resulted in lower cancer detection rates, particularly of early-stage disease, the team wrote. By the summer of 2020, these rates had generally recovered, but the recovery was uneven among various screening tests, including for lung cancer, and rates continue to be lower than expected, according to Doan's group.
"Delays in cancer screening can contribute to delays in diagnosis and increased deaths from cancer," the authors wrote.
The authors assessed how COVID-19 affected lung cancer (and mammography) screening via a study that included Medicare fee-for-service data from between January 2016 to February 2020 from 3.7 million men and women between the ages of 55 and 79 years; the team used this information to estimate expected screening rates for March 2020 to April 2022. Mammography screening rates were estimated from the same Medicare data set of a cohort of 1.6 million women between the ages of 50 and 74.
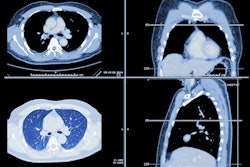
The investigators found an increase in low-dose CT scan rates for lung cancer screening between early 2017 and January 2020, from about 500 per million per month to 1,100 per million per month. But the pandemic changed this trend, "coincident with increases in national COVID-19 infection rates," the group noted.
From March 2020 to February 2020 and March 2021 to February 2022, observed lung cancer screening rates were 24% and 14% below what was expected. (On the mammography side for the same time frames, screening rates were 17% and 4% below expected, according to the authors.)
| Expected and observed lung cancer screening rates during the COVID-19 pandemic | |||
| Lung cancer screening rate (per 1 million Medicare beneficiaries) time frame | Expected | Observed | Percent difference |
| March 2020 to February 2021 | 14,939 | 11,411 | -24% |
| March 2021 to February 2022 | 17,666 | 15,201 | -14% |
The group also noted that factors such as low income (as determined by Medicaid eligibility) and race/ethnicity were associated with not only lower prepandemic screening rates for both lung and breast cancer, as well as with a decreased recovery of screening rates in March and April of 2020.
"Additional resources for specific initiatives targeting those populations are necessary," Doan and colleagues urged.
The study shows that the task of returning to pre-pandemic cancer screening rates needs some work, according to the investigators.
"In this cohort study, the decreases in cancer screening during the early phases of the COVID-19 pandemic did not resolve after the initial pandemic surges," they wrote. "Successful interventions to improve screening rates should address pandemic-specific reasons for low screening participation."
"More widespread recognition of the slow recovery from pandemic-related deficits in cancer screening should lead to more focused efforts to remedy the deficits," the group concluded.
Healthcare providers must work to make patients more aware of cancer screening, wrote Dr. Katherine Kahn of the University of California, Los Angeles, in a commentary that accompanied the study.
"Many opportunities are available to improve cancer screening and population health," she noted. "Evidence is increasing that implementing these changes to address both long-standing and more recent COVID-19-associated individual vulnerabilities and population vulnerabilities is both necessary and feasible."