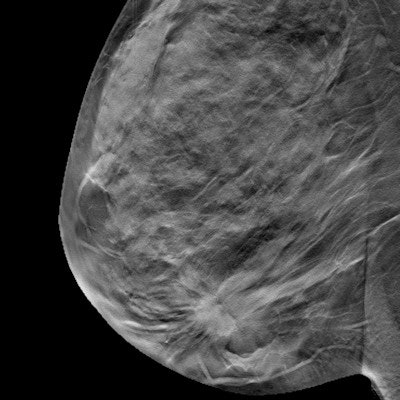
Adding digital breast tomosynthesis (DBT) to full-field digital mammography doesn't improve cancer detection metrics in asymptomatic women who are breast cancer survivors, a study published August 11 in Radiography found.
A team led by Emily Nia, MD, from the University of Texas MD Anderson Cancer Center in Houston found no evidence that the addition of DBT improves cancer detection rate, recall rate, or positive predictive value (PPV) in these women. The group also found no evidence of improvement when data were separated by age, race, and laterality.
"In general, although the imaging surveillance for asymptomatic women with a history of breast cancer is imperative, the addition of DBT ... does not statistically improve breast imaging metrics," Nia and co-authors wrote.
DBT continues to show promise in breast cancer imaging, with studies suggesting it outperforms conventional digital mammography and improves metrics such as cancer detection rate and recall rate. However, the researchers noted a lack of data in DBT's performance in breast cancer survivors. The few studies that have been published in this area reported that adding DBT to annual mammography screenings improves performance metrics.
Nia and colleagues wanted to compare the performance of 2D full-field digital mammography alone to full-field digital mammography plus DBT in surveillance imaging of asymptomatic patients with a history of breast cancer.
In their retrospective study, the researchers included data from 20,210 breast imaging exams. Of these, 7,235 were 2D studies and 12,975 were DBT (3D) studies.
The team found no statistically significant differences in cancer detection rate (CDR) (p = 0.38), recall rate (p = 0.087), or PPV (p = 0.74) between 2D and 3D exams. This trend was also seen when the data was stratified, with p-values exceeding 0.05 when exams were compared for fatty and dense breast tissue.
The researchers also found no significant differences in recall rate or PPV when data was stratified based on age. However, they found that cancer detection rate significantly increased in the 2D group (1.2%) compared with the 3D group (0.6%) for women ages 60 to 69 (p = 0.021).
The team also reported no significant differences in recall rate or PPV between the two groups when data were stratified by race. However, the 2D group experienced a higher cancer detection rate in white women compared with the 3D group, 6.7% versus 5% (p = 0.036).
Finally, the researchers found that the 2D group also experienced a significantly higher cancer detection rate when it came to unilateral studies, 0.7% versus 0.4% (p = 0.009). However, they did not find any significant differences in recall rate or PPV when data was stratified by laterality.
The study authors suggested that these results may be due to the work environment that the breast radiologists in the study practice in.
"We practice in a large tertiary cancer center where the majority of our patients are actively being staged for breast cancer or are survivors screened for their annual surveillance," they wrote. "Frequently imaging a patient population with complex pathology has resulted in radiologists with greater depth of experience and may potentially improve the overall ability to detect malignancy no matter the type of imaging utilized."
The authors also called for more studies in relation to screening regimens of breast cancer survivors.
The full study can be found here.