Combining ultrasound with MRI could help better differentiate between benign and malignant breast nonmass-like lesions initially detected on ultrasound, a study published October 12 in Ultrasound in Medicine & Biology found. Researchers led by Rui-Lan Niu, PhD, from the Chinese PLA General Hospital in Beijing, China, found that their combined method led to improved performance in this area over each modality alone.
“The study determined that the integrated diagnostic strategy had good performance in the diagnosis of nonmass-like lesions, which can improve diagnostic specificity while maintaining high sensitivity,” Niu and co-authors wrote.
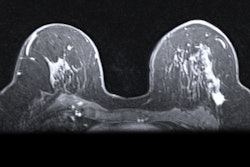
Some breast lesions do not meet the threshold for being classified as a mass. These are defined as nonmass-like lesions, which are areas of altered echotexture that differ from the surrounding breast tissue and do not conform to a mass shape. Differentiating between benign and malignant lesions in this area is important since various breast diseases can present as nonmass-like lesions.
Ultrasound and MRI have their tradeoffs in supplemental breast imaging. The researchers noted that many unnecessary biopsies of nonmass-like lesions are performed due to overlapping sonographic features of benign and malignant lesions, along with a lack of sonographic description and assessment in BI-RADS ultrasound. MRI, meanwhile, has high sensitivity but low specificity, which means BI-RADS 4 lesions may be subject to unnecessary biopsy.
The Niu team wanted to investigate the added value of MRI in assessing nonmass-like lesions detected initially on ultrasound. It also wanted to establish an integrated strategy of ultrasound combined with MRI to improve the diagnostic accuracy of nonmass-like breast lesions.
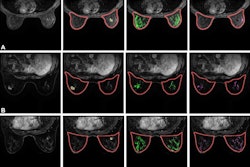
The team tested the method in a training set consisting of 180 patients with 183 nonmass-like lesions. Of the total lesions, 88 were benign and 95 were malignant. The external validation set meanwhile consisted of 61 patients with 61 lesions, including 30 benign and 31 malignant. The team obtained pathology results through surgical excision or ultrasound-guided core-needle biopsy.
The researchers found that for both training and validation sets, the combined method showed superior performance. This included increasing specificity while maintaining high sensitivity values.
| Performance of combined ultrasound, MRI method compared singular modalities | |||
|---|---|---|---|
| |
Ultrasound |
MRI |
Combined method |
| Training set |
|||
| Area under the curve (AUC) |
0.73 |
0.849 |
0.901 |
| Specificity |
52.3% |
75% |
87.5% |
| Sensitivity |
93.7% |
94.7% |
92.6% |
| Validation set |
|||
| AUC |
0.728 |
0.838 |
0.899 |
The researchers also found that for the training set, the combined method achieved statistical significance when compared to MRI or ultrasound alone for AUC and specificity values (p < 0.001 for both). For the validation set, the combined method was significantly better than ultrasound alone (p < 0.001), but not for MRI alone.
Additionally, the team reported that the false-negative rate seen in MRI for the study was 5.3% and that all falsely negative lesions were ductal carcinoma in situ (DCIS) without abnormal enhancement on MRI.
“The absence of abnormal enhancement may be due to the small size of lesions or the presence of moderate or marked background parenchymal enhancement [BPE],” it wrote.
The combined method led to two additional false-negative lesions. These were low-grade DCIS with small size and no typical malignant sonographic features, according to the researchers. It also correctly identified 11 false-positive lesions as benign lesions.
The study authors called for multicenter prospective studies that can control for confounding factors to further verify the value of the combined method.
The full study can be found here.