Imaging surveillance may be the way to go for monitoring radial scars without atypia found on screening digital breast tomosynthesis (DBT), research published March 13 in the American Journal of Roentgenology found.
In a study, Claire Crowley and Manisha Bahl, MD, from Massachusetts General Hospital in Boston, found that screening-detected radial scars without atypia at core-needle biopsy have a low upstaging rate to breast cancer of less than 2%.
“Our results, which show that surgical excision is not necessary for all patients with radial scars, could lead to a reduction in unnecessary surgery and could save patients from the morbidity and costs associated with surgery,” Bahl told AuntMinnie.com.
Radial scars typically present as architectural distortions on digital mammography. However, the researchers noted that these findings are becoming increasingly prevalent on screening DBT.
The recommended treatment option for radial scars is surgical excision due to “high and widely variable” reported surgical upstaging rates, the researchers explained. They also pointed out that universal guidelines for radial scar management in the current era of DBT are lacking.
Crowley and Bahl determined upstaging rates of screening DBT-detected radial scars with and without atypia and identified features related to upstaging risk. The retrospective study included women who underwent core-needle biopsy showing a radial scar after screening DBT and digital mammography between 2013 and 2020. It excluded women without surgical excision or at least two years of imaging follow-up after biopsy.
The team included data from 153 women with an average age of 56 years and with 159 total radial scars. Of the total scars, 128 underwent surgical excision while 31 underwent at least two years of imaging follow-up.
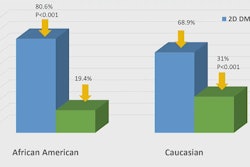
The researchers found that seven radial scars were upstaged to ductal carcinoma in situ (DCIS) while another was upstaged to invasive disease. This means the upstaging rate of the total radial scars was 5% (8/159). Also, the upstaging rates of radial scars with and without atypia at biopsy was 20% (6/30) and 1.6% (2/129, p < 0.001).
On multivariable analysis, the team reported that having a prior breast cancer diagnosis (62.5% vs. 4.8%, p = 0.01) and the presence of atypia on biopsy (75% vs. 15.9%, p = 0.02) were features linked to higher upstaging risk.
Finally, Crowley and Bahl found that the upstaging rate according to mammographic finding type was 7.1% (1/14) for asymmetries, 6.7% (1/15) for masses, 6.3% (6/96) for architectural distortion, and 0% (0/34) for calcifications.
The authors highlighted that their findings may collectively impact decision-making regarding radial scar management.
Bahl said the team is currently studying outcomes in patients who opt for imaging surveillance rather than surgery and determining optimal follow-up protocols for these patients.
“We are also interested in exploring the use of AI to help risk-stratify women with radial scars,” she told AuntMinnie.com.
The study can be found in its entirety here.