African American women are more likely to be recalled from a 2D digital mammography exam than from a digital breast tomosynthesis (DBT) exam, a study presented May 7 at the American Roentgen Ray Society (ARRS) annual meeting found.
In her talk, Brielle Paolini, MD, PhD, from the Medical University of South Carolina (MUSC) discussed her team’s results, which also showed that Caucasian women are more likely to be recalled from DBT exams. She also reported that architectural distortions and masses are more likely to be recalled from screening via DBT.
“Asymmetries were less likely to be recalled from screening via a DBT exam,” Paolini added.
While breast cancer mortality has declined in the past three decades since the widespread implementation of screening mammography, racial disparities in this area persist. African American women have a near-40% higher breast cancer mortality than Caucasian women and tend to be diagnosed with more advanced disease.
And while previous studies have highlighted that DBT leads to lower recall rates and improved cancer detection over conventional digital mammography, Paolini pointed out that women in minority populations are less likely to have access to the technology.
Paolini and colleagues conducted an institutional review with mammographic data collected between 2012 and 2020. They reviewed these data for mammographic findings, patient follow-up, cancer detection, breast cancer risk, and demographic variables such as age and race.
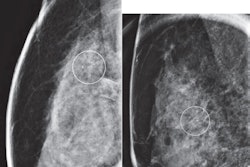
 Research presented at ARRS shows differences in recall rates for African American and Caucasian women who underwent DBT or 2D digital mammography.ARRS
Research presented at ARRS shows differences in recall rates for African American and Caucasian women who underwent DBT or 2D digital mammography.ARRS
The researchers reported that during the study period, 2,190 women were recalled from screening mammography. Of these, 568 (25.9%) underwent DBT while 1,622 (74.1%) underwent 2D digital mammography.
Also, of the total women, 1,191 (54.4%) were Caucasian while 912 (41.6%) were African American. Paolini said given this preponderance in the team’s dataset, the researchers chose to focus their analysis on these two patient cohorts.
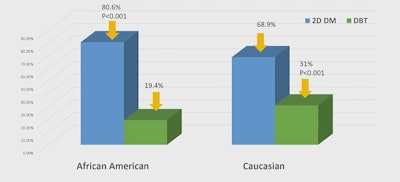
The team found that African American women were more likely to be recalled on 2D mammography while Caucasian women were more likely to be recalled from DBT.
| Comparison of recall rates between women undergoing DBT, 2D digital mammography | |||
|---|---|---|---|
| 2D digital mammography | DBT | p-value | |
| African American women | 80.6% | 19.4% | < 0.001 |
| Caucasian women | 68.9% | 31.1% | < 0.001 |
The study also included cancer risk data from 1,480 2D mammography patients and 531 DBT patients. Women who underwent DBT trended toward higher risk scores than women who underwent 2D mammography, but this did not achieve statistical significance (p = 0.1).
Additionally, more recalls from asymmetries stemmed from 2D mammography compared with those found on DBT (45.2% vs. 31.9%, p < 0.001). Meanwhile, more women who underwent DBT had architectural distortions compared with women who underwent 2D mammography (12.9% vs. 3.7%, p < 0.001). The same trend applied to masses found on DBT (24.1%) compared with 2D mammography (15.9%, p < 0.001).
“This makes me think that oftentimes, these focal asymmetries are getting recharacterized as masses once we introduce the 3D component,” Paolini said.
The team also reported no significant differences among diagnostic BI-RADS scores for both modalities (p = 0.36). The same trend went for cancer detection among 2D and 3D mammography types (p = 0.43).
Finally, while there was a trend for a higher percentage of invasive cancers diagnosed via DBT (75%) than 2D mammography (63.8%), this did not achieve statistical significance (p = 0.34).
Paolini called for future research to focus on identifying underlying racial, ethnic, and community barriers that decrease access to DBT screening. She added that such work could also make concentrated efforts to remove these barriers.
“At MUSC, we have a mobile mammography unit which travels to different sites throughout the entire state to try to help us improve access,” she said. “We also have staff whose job it is to reach out to patients who have been lost to follow-up in our system to try and recapture them into our system.”