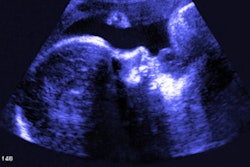
An abbreviated low-field-strength fetal MRI protocol can produce reliable structural and functional measures of the fetus and placenta in pregnancy, suggest findings published October 17 in Radiology.
Researchers led by Jordina Verdera from King’s College London in England found that the low-field-strength protocol showed significant correlations with MRI measures found in control groups, suggesting that the abbreviated protocol may perform as well as protocols using 1.5-tesla and 3-tesla MRI.
“These results offer the potential for increased patient accessibility because of shorter time requirements and a larger bore and allowed for wider use by reducing costs and removing the need for specialist techniques,” Verdera and co-authors wrote.
Previous studies suggest that low-field-strength fetal MRI has benefits for analyzing fetal development. These include reduced image artifacts, increased comfort, larger bore size, and potentially reduced costs. However, the researchers noted a lack of data in this area.
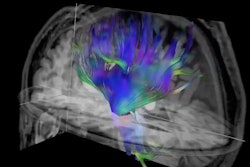
The Verdera team sought to explore the reliability and feasibility of low-field-strength fetal MRI for analyzing anatomic and functional measures in pregnant women. It used a commercially available 0.55-tesla MRI scanner (Magnetom Free.Max, Siemens Healthineers) and a comprehensive 20-minute protocol. The protocol included anatomic T2-weighted fast-spin-echo, quantitative T2, and diffusion sequences.
The researchers included data from 79 fetal MRI exams, with an average gestational age of 29.4 and an average maternal age of 34.4 years in 47 healthy pregnant women (control group), as well as in 32 participants with pregnancy-related abnormalities. They noted that the key anatomic 2D measures for the 47 healthy women agreed with large cross-sectional 1.5T and 3T control studies.
The team found that the interobserver correlations for the biparietal diameter in the first 40 consecutive scans were 0.96 (p = 0.002) for abnormalities and 0.93 (p < 0.001) for women in the control group.
It also found that functional features, including placental and brain T2 and placental apparent diffusion coefficient values, strongly correlated with gestational age. This included an average placental T2 in the control participants of 5.2 milliseconds of decay per week (R² = 0.66), and an average T2 at 30 weeks of 176.6 milliseconds (p < 0.001). The researchers noted that these values are “well within the range” for 1.5T and 3T MRI scanners.
Finally, the investigators reported that the women were more comfortable with the abbreviated protocol. On a 1 to 5 point scale, with 5 indicating “very comfortable” and 1 indicating “not comfortable,” survey respondents gave an average value of 4.3 for the low-field-strength scanner compared with 2.9 for the 1.5T and 3T scanners.
The study authors highlighted that their protocol has multiple advantages: reduction in the occurrence of artifacts, meaning reduction in time-consuming corrections; longer sampling along echo trains; and higher quality T2 data, increasing patient accessibility.
They called for future studies to have a dedicated high-risk study sample and additional fetal body anomalies, have paired participants who undergo both low- and high-field-strength exams on the same day, and analyze myelination.
“In addition, future work could focus on possible tissue contrast enhancement, perfusion techniques, and noncontrast-enhanced angiography, and may explore techniques and sequences exploiting the longer T2 and ability for longer readouts,” they wrote.
In an accompanying editorial, Penny Gowland, PhD, from the University of Nottingham echoed the Verdera team’s calls for more studies in this area. However, she also highlighted that the study is “an important step in establishing the sensitivity and efficiency of low-field-strength MRI, which will be important in selecting the right field for a particular scan.”
The full study can be found here.