Minnies finalists, page 2
Best Radiologic Technologist Training Program
Emory University, Atlanta, GA
Emory University's medical imaging program touts its high pass rate for the American Registry of Radiologic Technologists (ARRT) exam, with Emory graduates sporting a five-year average pass rate of 96.5% -- on their first try.
The program has similarly high standards for its job placement rate, with a five-year average employment rate of 94%. It typically enrolls an average of 10 students a year and offers four-year baccalaureate degrees, which helps graduates advance more rapidly within the radiologic technology profession.
Advanced coursework is offered in topics such as radiology administration and radiography education, as well as advanced clinical practice in CT, MRI, interventional radiology, and women's health including mammography and bone densitometry. The school's program director is Ted Brzinski Jr., who has been an instructor at Emory since 2008.
Thomas Jefferson University, Philadelphia, PA

Always a highly regarded program in radiologic technologist education, the department of radiologic sciences at Thomas Jefferson University (TJU) last won the Minnies award in this category in 2014.
One of the aspects that makes Thomas Jefferson's program unique is that graduates finish with a Bachelor of Science degree rather than the associate degree that's more common at other programs. The school believes having the more rigorous degree means graduates will be better prepared for working in today's healthcare environment, where the emphasis on quality requires staff members who are more credentialed and better educated.
TJU offers 10 tracks in imaging education, including radiography, MRI, CT, PET/CT, sonography, radiation therapy, and medical dosimetry, with each track taking a year to complete. A master of science program is also offered, which now includes a master in medical physics. The training reflects TJU's view on the typical employment experience for radiologic technologists today, which might find them working in radiography one day and MRI the next. The program is directed by Frances Gilman.
Most Significant News Event in Radiology
Arrival of artificial intelligence and machine learning in radiology
Artificial intelligence (AI) remains a red-hot topic in radiology. The subject was named the Most Significant News Event in Radiology in the 2016 Minnies awards, and it could repeat again in 2017.
Radiologists continue to be of two minds about AI and its related discipline, machine learning. On the one hand, many express trepidation that AI and machine learning will displace radiologists by taking over image interpretation tasks -- indeed, several articles in the lay press in 2017 identified radiology as one of the white collar disciplines that could be most threatened by the technology.
On the other hand, most of the leading minds in radiology believe that AI will serve in a complementary role to radiologists rather than a competitive one. In this view, AI will offer a helping hand to radiologists beset by growing scan volumes and external pressures.
European regulators propose pulling linear gadolinium contrast from market
The issue of gadolinium retention in patients receiving MRI contrast had been percolating for several years when European regulators dropped a bombshell in March, recommending that four gadolinium-based contrast agents (GBCAs) be pulled from the market: MultiHance, Omniscan, Magnevist, and Optimark.
The recommendation by the European Medicines Agency's Pharmacovigilance Risk Assessment Committee (PRAC) stunned industry observers who had been following the gadolinium retention issue closely. While numerous clinical studies have shown that retained gadolinium remains in the brains of patients for as long as years after they receive MRI contrast, no study has demonstrated any clinical impact from the phenomenon -- at least, not yet.
The PRAC in July amended its decision to state that MultiHance should remain in use for some liver imaging applications, but the other three agents remain on the chopping block. All four agents are linear GBCAs, which are considered to be less stable than macrocyclic agents and thus more prone to gadolinium deposition.
As researchers strive to learn more about the biological mechanism behind gadolinium deposition, the U.S. Food and Drug Administration played catch-up with European authorities by convening an advisory panel meeting on gadolinium in September. The group recommended that new text on gadolinium retention be added to the warning label of GBCA products on the U.S. market, and it voted to require that MRI contrast manufacturers conduct new studies on safety.
Biggest Threat to Radiology
Commoditization of radiology services

This has become a perennial topic of concern to radiologists, and as such it has been named as the top threat to radiology by the Minnies expert panel for the past three years running.
Driving the concern has been economic pressure being exerted throughout the healthcare system. But some trends are peculiar to radiology, such as the growing consolidation of group practices into larger entities. And teleradiology is still viewed askance by many more traditional radiologists.
Even farther in the future, artificial intelligence (see below) threatens to put radiologists in competition not only with other radiologists but also with machines (assuming you're a skeptic about AI's future trajectory).
On the other hand, there has been no visible erosion in radiologist salaries, with the median radiologist salary in the U.S. topping $500,000 for the first time in July in a survey by the American Medical Group Association.
So maybe there's nothing wrong with being a commodity -- as long as you are a well-compensated one.
Use of artificial intelligence to interpret medical images
Several years after its arrival in radiology, radiologists are still struggling to adapt to artificial intelligence -- or rather, the idea of artificial intelligence. AI technology is still mostly a research tool that has yet to make prominent inroads into clinical practice.
But AI still scares the pants off radiologists. To confuse matters, radiologists have been treated to dueling headlines over the past year. Articles in the lay press have predicted the looming demise of radiologists, with computer scientist Geoffrey Hinton predicting in October 2016 that AI algorithms will make the specialty obsolete in five to 10 years -- and we should stop training radiologists now, he believes.
But soberer minds offer a less histrionic future, one in which humans and machines work together to deliver better healthcare to patients. These industry observers believe that radiologists should embrace AI so that they are the ones who control it when the technology rises to its full potential.
Hottest Clinical Procedure
3D printing of internal anatomical structures
 Image courtesy of UCSD.
Image courtesy of UCSD.Winner of the Minnies award for Hottest Clinical Procedure in 2016, 3D printing shows no sign of cooling off. Indeed, the past year has seen heightened interest in the technology as a tool for a variety of clinical and educational tasks.
The 3D printing segment even got its own annual event with the 3DHeals conference in April in San Francisco. The meeting explored multiple aspects of the discipline, ranging from legal issues to challenges facing 3D printing start-ups.
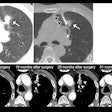
Among notable clinical developments in 2017, researchers from Northwestern University took the step of 3D printing functional organs in a mouse model, while a group from the University of California, San Diego (UCSD) explored the use of 3D-printed models to plan hip surgeries. And 3D prints aren't just useful for devices to be implanted in patients: A group from Brigham and Women's Hospital used 3D printing to create custom-printed tools for interventional radiologists to use during procedures.
Look for more exciting developments in the field of 3D printing in the coming year.
PET/MRI
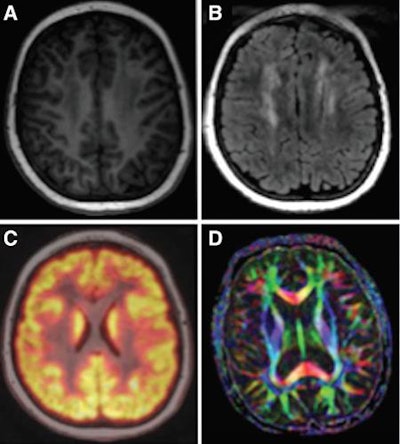 Image courtesy of Radiology.
Image courtesy of Radiology.Compared with 3D printing, PET/MRI is a relatively mature technology. But it continues to capture the imagination of radiology with its powerful fusion of functional information from PET with anatomical detail from MRI.
In 2017, researchers produced papers that demonstrated their effort to make the expensive technology more suitable for routine clinical imaging. For example, in August a group from Stanford University revealed a protocol for performing PET/MRI in a single session for pediatric cancer patients -- making the studies more tolerable. And in April, a German group found that using a lower dose of FDG didn't compromise the diagnostic quality of the PET component; meanwhile, another German group found PET/MRI to be no better than PET/CT for evaluating head and neck cancer.
At RSNA 2016, a group from NYU Langone Medical Center found that including the head in a whole-body PET/MRI scan uncovered more incidental findings that might have been missed -- with lower radiation dose than PET/CT. And a group from New York University found the modality to be well-suited for finding distant metastases in patients with breast cancer.
In the coming year, look for researchers to continue to refine PET/MRI to make it more economical and clinically useful, particularly for oncology applications.
Previous page | 1 | 2 | 3 | Next page