The future of imaging is three-dimensional. Although it first came on the scene with the introduction of CT scanning in the late 1970s, perceptions that 3D had limited clinical application and little emphasis by the major vendors kept it out of the limelight. Now it's taking center stage, creating images that radiologists could only dream of decades ago.
Taking data from cross-sectional CT and MRI studies, 3D technology creates spatial views of organs and systems, allowing physicians to visualize a patient’s anatomy realistically. Multiplanar reconstruction (MPR) review is now becoming the standard of care for interpretation of multidetector CT (MDCT) studies.
The 3D medical imaging world is in transition, according to Robert Taylor, chief operating officer for TeraRecon in San Mateo, CA. "There is a lot more to advanced postprocessing than just 3D, but most people use this term when referring to advanced visualization, measurement, and reformatting procedures performed by workstations that also feature 3D rendering," he said.
There are several approaches to 3D processing. The first real volumetric 3D productivity tool for physicians came in 1998 from Vital Images of Plymouth, MN. Now, five years later, 3D has become clinically accepted enough for scanner manufacturers to routinely include stand-alone 3D workstations as part of CT or MRI sales. They are ideally suited for research and offer the widest variety of functions, but can be expensive and difficult to use.
Other standalone workstations produced by non-scanner manufacturers, such as TeraRecon and Vital Images, are often less versatile but easier to use. And PACS vendors are beginning to offer 3D functionality directly on PACS workstations.
Products from software-only 3D providers (e.g., Voxar of Edinburgh, Scotland or Able Software of Lexington, MA) can be loaded on standard PCs to produce powerful stand-alone workstations, or they can be loaded directly on PACS workstations to enhance 3D functionality directly in reach of the radiologist.
"This (type of) software offers the best of both worlds -- standalone and integrated PACS solutions -- so there is functionality as well as ease of use," said Dr. Matthew Barish, assistant professor of radiology at Harvard Medical School and director of the 3D and Image Processing Center at Brigham and Women's Hospital in Boston. "This is likely to be the number-one reason why this method of delivery of 3D is the fastest-growing sector of the market." (Barish is also chief medical advisor for Voxar.)
The data dilemma
The increasingly popularity of 3D is directly correlated to the explosion of data being produced by modality scanners, in particular CT. The newer multidetector CT scanners can produce as many as 5,000 slices per study at 0.5-mm thickness. The radiologist is then faced with a dilemma: View a subset of the data and lose the benefit of the MDCT scanner, or review all the images and lose time.
Cross-sectional scans can be "summarized" by 3D viewing, reducing the number of images that require review. MPR review increases lesion detection, reduces the number of images to review, and provides images that are easier to interpret by referring physicians.
MPR gives an oblique plane through a volumetric dataset that the radiologist can control arbitrarily to view structures out of the plane of the original 2D slice images acquired by the scanner. In addition to more-accurate diagnosis, 3D enables noninvasive surgical planning, resulting in reduced operating time and less damage to healthy tissue when the target area is isolated.
Rendering speed has been a problem, particularly with software-only 3D packages. But vendors are loading better software on newer and faster computer processors, resulting in marked improvement in rendering and segmentation processing.
Many observers believe the future of imaging revolves around direct 3D viewing replacing axial CT-scanned images, which means more radiologists will have to be trained in 3D rendering. This is a problem at some large medical centers, where specialization leaves residents without much hands-on training in 3D techniques.
Applications
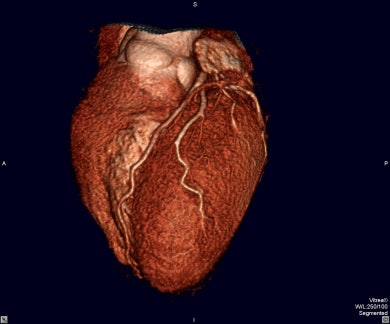
In neurosurgery, 3D visualization of cerebral vasculature from CT angiography aids surgical planning for aneurysms, allowing surgeons to spare crucial cortical areas and reducing operating time.
Orthopedics can utilize 3D not only in surgery but in the emergency department, where it helps surgeons understand skeletal trauma, particularly of the pelvis, shoulder, spine, or face.
Vascular surgeons use 3D angiography and multiplanar views to design aortic stents.
Gastrointestinal and genitourinary surgeons find 3D helpful in planning for pancreatic or renal tumor resection by analyzing vascular involvement. CT virtual colonoscopy and CT urography are being studied for future routine clinical use.
Thoracic surgeons are using CT angiography (CTA) to assess lung anatomy. Lung specialists are beginning to explore the use of computer-aided detection (CAD) software for use with 3D CT to detect lung cancer.
Ultrasound 3D is becoming more like CT and MR. It is used mainly for thyroid, pelvic, and abdominal exams, where bones don’t interfere. After the sonographer sweeps the probe across the patient, the information can be stored and recreated in a 3D dataset. The sonographer shoots several representative static pictures, and the radiologist can later read 3D renderings from any arbitrary view. One practitioner said it's like watching a movie -- reprobing data as though the patient is right in front of you.
With this technology, patients can be scheduled in off hours and off-site, without having a radiologist present to check each scan, which cuts down on scheduling wait time as well as scan time.
Integration with PACS
Many radiology practices still use modality workstations for 3D viewing and reconstruction, but more and more facilities are integrating 3D functionality within their PACS viewing workstations, giving radiologists immediate access to maximum intensity projection (MIP) and MPR functions and advanced 3D tools.
A facility’s PACS gives easy access to 3D studies. Trained radiologists or technologists render 3D images from CT and MR studies and return them to the PACS, where they can be archived with 2D cross-sectional images of a case and retrieved for viewing. Physicians can access the studies from a facility’s servers with privacy-protected software from their home PCs.
As more and more referring physicians are granted limited access to PACS networks, 3D images are simply becoming part of the patient’s standard DICOM image set. These images are then available over a PACS Web connection to referring physicians. Although some radiologists are still forwarding 3D reports on film, others are using HIPAA-compliant e-mail, CD-ROMs, or DVDs.
Hardware or software?
Workstations are often installed as a package with scanners. If you have a PACS, you need to be able to send the rendering results back to the PACS, and be able to retrieve them at will. Basic scanner packages might only offer MPR and MIP functionality.
Discussing the various options for 3D, Dr. Christoph Wald, director of Advanced Image Analysis and Virtual Surgical Planning at Lahey Clinic Medical Center in Burlington, MA, suggested that community hospitals should go with the simplest and least-expensive solutions.
"If I were a small-town radiologist, the one thing I’d be looking for would be a PC-based, simple, versatile tool such as the Voxar," Wald said. "If you have a PACS, you definitely want an integrated solution, where you don’t need a stand-alone workstation, but where you actually have it integrated in your PACS by the push of a button."
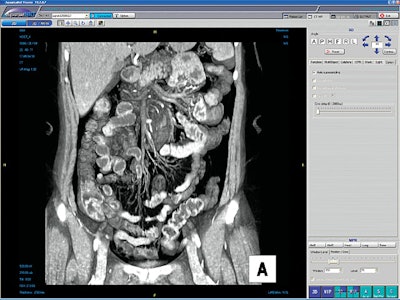
If you have a PACS network, Wald said, you already have a way of scrolling through MDCT images quickly, which is better than having 20 or more sheets of film, but if you have a 3D workstation on top of that, "not only can you scroll through this stuff, but you can actually look at it in a coronal image, or a sagittal image, or a volume-rendering image, or a MIP image. Those sometimes put things together in a different way.
"Your brain suddenly understands: ‘Oh, yeah, there’s a small artery I didn’t pick up on because it was just a little white wandering dot that’s moving through the axial images as you scroll through them. If you don’t scroll through them, you won’t be able to pick it up at all. That little dot you didn’t see might be a significant artery."
Able Software and Voxar market software-only products. Several other companies do likewise, but sell to OEMs for installation on scanners.
Return on investment
Trying to justify 3D hardware and software purchases is not as clear-cut as it might be for CT or MR scanners, for example. The return on investment is more difficult to assess. Most new scanners have 3D capability built in, as do most PACS networks. But trying to pay for add-on 3D capability may require creativity, as the reimbursement climate doesn’t currently recognize the way 3-D is used.
Purchasing 3D software for one or two PACS stations would mean buying one or two licenses for a retail price of $25,000 to $30,000 apiece. Workstations cost from $30,000 up to $100,000, not a major expense for most facilities.
But for reimbursement, there is only one CPT code (76375) for 3D processing. Depending on whether you’re billing as a hospital-based or as a nonhospital facility, Medicare pays about $100 for hospital-based and $150-$170 for non-hospital-based 3D exams. Gordon J. Harris, Ph.D., director of the 3D labs at Massachusetts General Hospital (MGH) in Boston, said his lab was funded by MGH’s physicians’ organization, so they bill through that group as a nonhospital facility.
Until two years ago, you could use the 76375 CPT code whenever you did any kind of 3D processing. However, CMS has changed its reimbursement policy and has made 3D processing a mandatory part of MRA (magnetic resonance angiography) and CTA.
CTA until 2001 was considered a CT-plus-3D reconstruction, and was billed with a multiprocedure code. CMS took this opportunity to bundle the codes for CT and 3D for those procedures, because a facility would always do 3D with a CTA. They created new CTA codes.
For instance, CMS said 3D is such an integral part of doing CTA that it can’t be charged for separately. So the agency raised the CT reimbursement rate by $5, causing facilities to actually lose $95 over the previous schedule. Essentially the same situation exists for MRA.
As one radiologist said, only half in jest, if you’re charging Medicare for a CT angiography and you’re not doing 3D, you’re basically committing fraud.
A group of radiologists and lab directors, the American College of Radiology (ACR), vendors, and contrast developers are lobbying CMS to change the CPT codes, arguing that such low reimbursement is a roadblock to 3D development because it doesn’t reflect the reality of expense and time in using the technology. The group hopes to effect reimbursement changes in a year or so.
CTAs and MRAs have largely replaced catheter angiography at MGH, Harris said, so it’s not only cost-effective in time and materials, it also exposes patients to less risk. But as Medicare rates don’t reflect the work involved, hospitals are losing money. A traditional catheterized angiogram pays $5,000, while a CTA pays $300.
MGH does about 60% of its 3D rendering for MRA and CTA. The other 40% is orthopedics, neurology, and other applications, so the hospital can apply the $100 or $150 reimbursement for those other procedures. Thus, if a facility spends less than $100,000 and gets several low-end workstations, or one high-end one, it probably would recoup the investment in a short time.
"You have to be able to persuade the hospital that you’ll do a better job of the CTAs and MRAs if you have somebody who is dedicated to doing 3D, and if you have a workstation to do it on," Harris said. "In these times it’s hard to make an argument without an ROI."
Conclusion
Radiologists often say they can make a diagnosis on an axial 2D image, but MPR is becoming the standard of care. And the challenge is even greater for surgeons. Unlike the radiologist, the surgeon must sit down with his or her patient and explain what he or she proposes to do in the operating room. The surgeon has to convince the patient that the proposed procedure is best for him or her.
As Christoph Wald said, "You have no idea how powerful it is for surgeons to have one image that shows the aneurysm or the tumor, and say to the patient, ‘Look, here it is. This is what it looks like. This is what I need to get at.’ The traditional drawing surgeons make for patients has been replaced by powerful imagery. Surgeons love it.
"It’s almost arrogant for the radiologist to say, ‘Oh, I can make that diagnosis on the axial image.’ We’re consultants. We have an obligation to those who come to us for consultation, to use the results in the way they should be used."
By Robert BruceAuntMinnie.com contributing writer
November 3, 2003
Related Reading
3D imaging in Europe: The jewel in the crown, May 30, 2002
Report forecasts strong growth in 3D market, April 24, 2001
A list of the 3D stories AuntMinnie.com has done:
Copyright © 2003 AuntMinnie.com