According to the preliminary results of the ACRIN 6666 trial, ultrasound boosts cancer detection but at the risk of a higher false-positive rate. While the trial investigators continue to mine the trial data to find the best place for the modality in a screening setting, other researchers are adding performance-enhancing bells and whistles to breast ultrasound.
First, one radiologist found that 3D automated breast ultrasound (ABUS) helped identify and localize breast lesions that were missed by conventional technologies. In a second paper, a San Diego-based group tested a computer-aided sonographic imaging analysis tool to compare reader results.
ABUS localizes breast cancers
ABUS exams changed the surgical management of 8% of women enrolled in the first study led by Dr. Jessica Guingrich.
"Three-dimensional images enabled discovery and treatment of malignant breast lesions which had not been detected using a conventional protocol that included mammography, handheld ultrasound, and MRI," said Guingrich, who is the medical director of breast imaging at the Susan G. Komen Breast Center and the Centers for Breast Health at OSF Saint Francis Center, both in Peoria, IL. She is also a medical adviser for U-Systems of San Jose, CA, which manufactures the SomoVu unit used for this research.
The patient population consisted of women who were scheduled for screening or diagnostic ultrasound exams between September 2005 and March 2007. Most (70%) had been referred for ultrasound screening because of dense breast tissue, Guingrich stated.
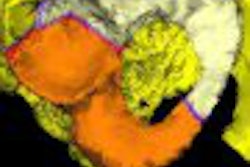
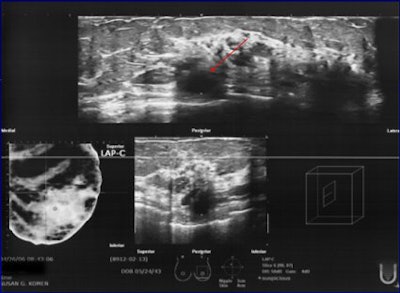
 |
| 62-year-old patient underwent bilateral screening mammogram and was called back for additional imaging of a posterior left breast asymmetry and anterior left breast calcifications. On ABUS, the first diagnosed left breast cancer can be seen at 12 o'clock, 3 cm from the nipple, corresponding to site of subareolar calcifications seen mammographically (infiltrating ductal carcinoma). |
The subjects underwent mammographic exam, handheld ultrasound exam (HHUS), and ABUS studies. In some cases, MRI was done as well. The study group was then parsed down to only those patients whose findings were categorized as BI-RADS 3-6. Visibility of these lesions on ABUS was then compared to the other modalities.
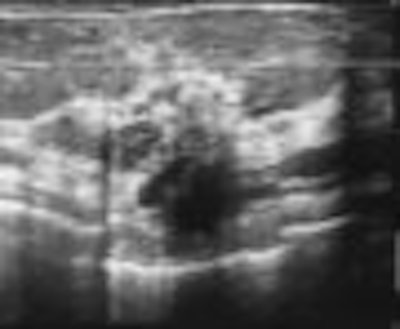
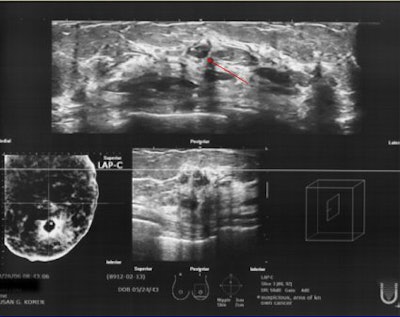
 |
| Same patient as above. Second left breast cancer at 10 o'clock, 2 cm from the nipple was found on ABUS (and not seen on initial hand-held ultrasound exam), which corresponded to the posterior mass demonstrated mammographically and on breast MRI. Images courtesy of Dr. Jessica Guingrich. |
A total of 748 breasts in 429 patients underwent ABUS imaging. A subset of 146 patients was categorized as BI-RADS 3-6. Within this group, 117 biopsies were performed after which 45 cancers and 72 benign lesions were found. In 17 cases (13 multicentric or multifocal lesions; three bilateral cancers), the cancer was confirmed with biopsy prior to the ABUS exam and assigned a BI-RADS 6.
Among the 117 biopsied lesions, 46 were not seen on mammography. Among 149 HHUS cases, four cancers were missed on the first attempt. One cancer was missed on 24 MR studies. Among these missed lesions, ABUS demonstrated a second cancer not seen on MRI, a mammographically occult contralateral cancer, and one cancer not seen on first-attempt HHUS.
Computer-aided imaging system
In a second RSNA presentation, researchers from the University of California, San Diego (UCSD), discussed their experience with an in-house, experimental ultrasound computer-aided imaging system called Breast Companion.
"A computer-aided tool for breast diagnosis is needed because diagnosis is difficult to perform and interpret due to variability between readers and operators," said Michael Andre, Ph.D., an adjunct professor at UCSD and the San Diego Veterans Affairs Medical Center in La Jolla, CA. Andre is also an advisor to Techniscan Medical of Salt Lake City, which markets an ABUS system.
The Breast Companion measures lesion margins, shape, echogenicity, echo texture, orientation, density, and posterior acoustic pattern, Andre explained. The system identifies a lesion, measures nine lesion characteristics, compares those characteristics to the reference library, and selects seven comparative masses. These are then displayed for the radiologist to review during interpretation.
The reference database was populated with 21% malignancies, 36% solid benign tumors, 12% complicated cysts, and 29% simple cysts.
For this study, Andre's group looked at the following:
- Performance of Breast Companion with three independent sets of cases
- Inter- and intraobserver variability among four reading the same set of cases
- Breast Companion performance using a reference template with a decreasing number of cases
According to the results, the area (Az) under the receiver operating characteristics (ROC) curve for Breast Companion in a 329-case set was 0.96. In a 595-case set and a 925-case set, the Az was 0.98. On the same cases, the Az for the four radiologists ranged from 0.90 to 0.83. Observer variability was comparable. Andre said that a case set of 595 cases was sufficient "for us to detect a 10% difference in specificity and a 5% difference in sensitivity."
Andre said the Breast Companion imaging system, which the group has been working on for two years, could be ready for field testing in 2008.
By Edward Susman
AuntMinnie.com contributing writer
December 26, 2007
Related Reading
New techniques in breast ultrasound may find more cancers, March 1, 2007
Automated breast US proves to be sensitive screening tool in dense breasts, November 29, 2006
Auto breast US handily spots lesions in early study, January 13, 2006
Copyright © 2007 AuntMinnie.com