From its roots in 1980 as a novel idea for speeding up product design and prototyping, 3D printing has grown into a cottage industry in healthcare, finding myriad roles in patient care and physician training, according to a review article published online May 27 in the Journal of the American College of Radiology.
Medical applications for 3D printing range from orthopedic devices to complex reconstructions of anatomy that allow operative planning and education for doctors and surgeons, wrote Dr. Anthony Trace, PhD; Dr. Daniel Ortiz; Dr. C. Matthew Hawkins; and colleagues from Eastern Virginia Medical School, the University of Virginia, Emory University, and other centers.
"In the contemporary climate of personalized medicine, the utility of tangible 3D models extrapolated directly from patient imaging data seems boundless," they wrote (JACR, May 27, 2016).
Radiology's new industry
The ability to perform presurgical planning is probably 3D printing's greatest accomplishment to date, while the ability to show patients 3D renderings of parts of their body has added an important benefit that didn't exist previously, wrote Hawkins in an email to AuntMinnie.com. Hawkins is a pediatric radiologist at Children's Healthcare of Atlanta at Egleston.
"Ultimately, 3D printing will open new doors in healthcare that we can't yet imagine," Hawkins said. "It is another way that we can begin to achieve true, personalized healthcare."
In their review article in JACR, Trace, Hawkins, and colleagues outlined the development of 3D printing, discussed its applications across several medical and surgical specialties, and addressed the obstacles and opportunities that radiology faces as it works to integrate the new 3D printing technologies.
The rapid prototyping concept behind 3D printing was first developed in Japan; in the U.S., the concept was advanced with the development of stereolithography. Over the next several decades, inkjet printing, laser sintering, laminate object production, and fused deposition modeling came into being, and these technologies form the foundation of today's 3D printers. There are many ways to convert digital information into a physical object, the authors wrote.
"Computer-aided design (CAD) software translates a digital model into a series of polygons, usually triangles, the number of which directly correlates with resolution," they wrote. "3D printers translate these data into dimensional planes that, in consecutive series, serve as the construction template for the production of a physical model. Extrapolating DICOM datasets entails a similar progression."
DICOM data can be extracted from image files using any number of open-source software programs (such as K-PACS), or the information can be uploaded directly to surface rendering software such as Matlab or FreeSurfer. The programs isolate an anatomic surface or extract a region of interest and convert the data into a stereolithography (STL) file, the most common 3D file format. The data can then be manipulated and sculpted using free software options such as Blender and Meshlab, or high-end 3D animation and modeling software programs such as Autodesk Maya and ZBrush.
STL files can be used by most printers, making DICOM data a viable bridge linking 3D printing technology with patient-specific data. A complete guide to 3D printing by Naftulin et al was published in 2015 in PLOS One, the authors noted.
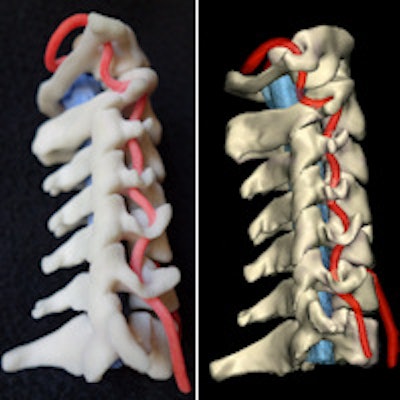
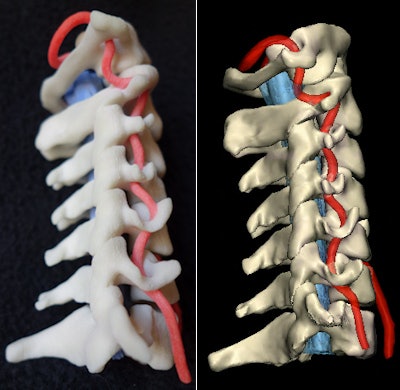 Physical 3D-printed multicolor nylon model (left) demonstrating the cervical vertebrae, vertebral arteries, thecal sac, and cord. Virtual version (right) of the printed model shows the same structures. 3D printing by WhiteClouds in Ogden, UT. Images courtesy of Dr. Justin Cramer and Dr. Edward Quigley, PhD.
Physical 3D-printed multicolor nylon model (left) demonstrating the cervical vertebrae, vertebral arteries, thecal sac, and cord. Virtual version (right) of the printed model shows the same structures. 3D printing by WhiteClouds in Ogden, UT. Images courtesy of Dr. Justin Cramer and Dr. Edward Quigley, PhD.Healthcare in 3D
3D printing has shown value in several areas of medicine, ranging from training and patient education to diagnostic and therapeutic applications. Reports of its use come from neurology, cardiology, and interventional radiology, along with many other subspecialties, Trace and colleagues wrote.
Preoperative planning has been a key area of early implementation, enabling providers to pare back on time-intensive clinical trials and the use of laboratory animals with reconstructions of highly complex patient anatomy. Independent studies have shown that models save intraoperative time, enhance clinical outcomes, and reduce complications, the authors wrote.
In prosthetics, the one-size-fits-all approach for devices is giving way to personalized medicine, reducing costs and fabrication time for personalized prostheses with rapid, low-cost production. Dental and maxillofacial surgical centers in China are using 3D printers to create patterns for nasal and other facial prosthetics. The volunteer organization e-NABLE has developed an open-source forum for the design, development, and sharing of computer-aided design files for the construction of prosthetic hands.
Advanced 3D printers are capable of depositing multiple solid substrates, such as plastic and metal, to create 3D models, as well as water-soluble substrates, enabling highly detailed moving components that have no need for additional assembly because unnecessary intervening materials can be washed away after production.
The paper's authors have experience in integrating 3D model production to reduce prosthetic turnaround time for veterans with below-the-knee amputations in a process that involves transferring STL files directly to 3D printers.
In patient education, 3D models can impart understanding in tactile ways that written reports cannot communicate, the group wrote. In graduate medical education, 3D printing has been used to create patient-specific scenarios, helping trainees better understand each patient's anatomy and anticipate challenges in a low-risk environment.
"3D printing may also improve radiology's involvement in patient care by reproducing 3D models used to educate other clinicians at multidisciplinary conferences," Trace and colleagues wrote. "This would enable clinicians and surgeons to better understand patient anatomy and the relation of disease to unaffected tissue, and would ultimately allow radiologists to potentially add value to patient care."
Challenges ahead
Getting reimbursement codes for 3D printing will be crucial to the industry's long-term success. A solid precedent for reimbursement has already been established with the approval of reimbursement codes for 3D imaging reconstructions: 76376 and 76377.
These are differentiated based on where the reconstruction was performed -- at the scanner or at the workstation. Both require "concurrent physician supervision," which includes design of the anatomic region to be reconstructed, determination of tissue types and structures to be displayed, determination of images or cine loops to be archived, and monitoring and adjustment of the 3D product.
One of the greatest potential perils for 3D printing is the disparate regulation and practice guidelines that might develop if it is implemented haphazardly by multiple subspecialties throughout healthcare systems, Hawkins said.
"This is why radiology, which generates the data that create 3D-printed objects, should take the lead in developing regulatory and reimbursement policies for this technology," he said.
Radiopharmaceuticals provide a logical precedent for the regulation of 3D materials, the authors wrote. For example, radioisotopes are produced at manufacturing facilities that follow one set of regulations and are used by nuclear medicine facilities that have a different set of rules.
3D printing needs radiology
Without a single, central specialty taking the lead in implementing the technology, 3D printing's integration will be exposed to inefficiencies and potential disorganization as multiple specialties attempt to implement similar processes simultaneously.
Radiology must decide its role in the clinical workflow of 3D printing, and that means the specialty must decide whether to lead or to follow. As the universal hub for image acquisition and storage within hospitals and healthcare systems, radiology is appropriately positioned to administer and refine 3D printing processes, according to Trace and colleagues.
Alternatively, hospitals might lead the development and implementation of 3D printing, but the result would be geographically variable adoption and challenges in the development of universal protocols, guidelines, and best practices.
"Radiology, as a profession, should thus seize this opportunity to lead healthcare and all medical specialties into the 3D printing era," the authors concluded.