Even experienced nephrologists can improve their preoperative planning when 3D-printed kidneys are available, according to the results of a new study in Abdominal Radiology. 3D models can shift some surgeries to less-invasive options after the translucent printed models are used for planning.
Researchers from New York University School of Medicine created 10 3D-printed kidney models for use in preoperative planning in patients with renal masses. The investigators created their surgical plans from imaging alone, then again after the use of a 3D-printed model for each case. They found that the planned intervention changed in each case, significantly in several cases.
"Our results showed that decisions regarding the planned surgical approach for renal cancers could be impacted with the 3D-printed models," lead investigator Dr. Nicole Wake told AuntMinnie.com. "We believe that facilitating better preoperative planning for renal cancers through the use of 3D-printed models may allow for fewer changes to be made in the operating room, which may reduce duration of induced ischemia or complications related to complex tumor anatomy."
Sparing kidney function
For decades, surgeons have relied on radical nephrectomy to treat renal masses, but the need to spare kidney function to the extent possible has led to the development of minimally invasive approaches that have narrowed the indications for radical nephrectomy, the authors wrote. Kidney-sparing surgeries are now used routinely through both open and minimally invasive techniques.
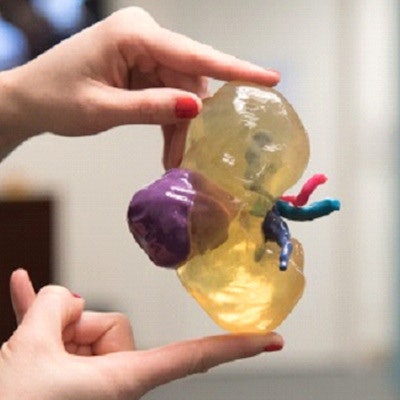
 3D-printed kidney. Image courtesy of Dr. Nicole Wake.
3D-printed kidney. Image courtesy of Dr. Nicole Wake."The decision to perform a partial nephrectomy, and the choice of which surgical approach to take, involves a complex interaction between various patient factors (e.g., comorbid conditions, age, and body habitus) and renal tumor morphology," they wrote (Abdom Radiol, January 7, 2017).
Among the factors that affect surgical planning and decision-making are the anatomic relationship of the tumor with other structures and its location within the kidney, the authors wrote. Here the use of 3D printing can potentially go beyond the ability to visualize the anatomy with 3D imaging alone.
Wake and colleagues sought to determine whether patient-specific 3D-printed renal tumor models created from MR images changed preoperative planning decisions made by urological surgeons in preparation for complex renal mass surgical procedures.
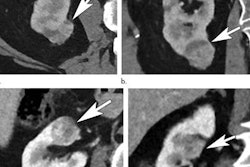
They examined 10 renal mass cases from a larger study -- all scoring less than 5 on the nephrometry score (a descriptive renal anatomy scoring system used to assess tumor complexity and to guide the surgical approach for renal tumor surgery).
Although CT images are generally used for 3D-printed models, the researchers considered MRI a better alternative in the kidney owing to better soft-tissue characterization and flexible image contrast mechanisms, as well as the lack of ionizing radiation.
MR images were acquired on a 1.5-tesla MR system (Avanto, Siemens Healthineers) using a postcontrast fat-suppressed gradient-echo T1-weighted sequence and spatial resolution of 1.4 mm x 1.4 mm x 2 mm. Postoperative images using the same parameters were acquired six months later. The images were processed on a dedicated software platform (Mimics, Materialise), which was used for 3D visualization, segmentation, and generation of stereolithography (STL) files.
The tumor, kidney cortex and medulla, main renal artery, main renal vein, and ureter were segmented as separate anatomical regions of interest (ROIs). Manual thesholding and editing were performed to ensure correct selection of anatomy. Each ROI was converted into a separate 3D object to create a 3D virtual model.
Printing materials included a clear, transparent flexible material (HeartPrintFlex, Materialise) and different combinations of rigid cyan and magenta (Stratasys) used on a Connex 500 printer (Stratasys). A measurement phantom was created using computer-aided design (CAD) software to ensure accurate measurement.
"The translucency of the 3D-printed models allows easy visualization of the location and size of the tumor as well as the relationship of the tumor to key anatomical structures such as the renal artery and renal vein," the authors wrote.
The models allow surgeons to touch the tumor and parenchyma, improving their understanding of the anatomy and therefore surgical planning.
Preplanning with and without
Three experienced urologists reviewed each renal mass case individually and in random order to plan an intervention first based on images alone, and once again based on images and the 3D-printed models. The urologists completed questionnaires about their surgical approach and planning, comparing presumed preoperative approaches with and without the model. In addition, they recorded any differences between the plan and the actual intervention.
The results revealed a change in the planned approach in all 10 models, with the largest impact of the models seen in decisions regarding transperitoneal or retroperitoneal approach and clamping, which changed in 30% to 60% of the cases. Major changes using the 3D model, compared with conventional image interpretation on PACS, were as follows:
- Partial or radical nephrectomy: One surgeon changed the potential surgical approach in one (10%) case and a second surgeon changed the approach in two (20%) cases.
- Open or laparoscopic approach: Two of the three surgeons changed their approach in one case (10%) each.
- Transperitoneal or retroperitoneal approach: One surgeon changed the approach in four cases (40%), and two surgeons changed the approach in three cases (30%) each.
- Clamping approach: One surgeon changed the approach in five cases (50%), and two surgeons changed the approach in four cases (40%) each.
"Our results indicate that even experienced urologists may potentially benefit from the 3D-printed models for planning of complex surgeries," the study team wrote.
In fact, the use of preoperative 3D-printed renal mass models could promote nephron-sparing surgery and preservation of healthy parenchyma, as surgeons gain a better understanding of the size and location of a tumor in relation to normal tissue and vital structures such as the arteries and veins.
Image postprocessing required about seven hours for each kidney model, and each took about 10 hours to print and cost about $1,000.
"Although this is currently time-consuming and expensive, image postprocessing times, printing times, and printing costs are all expected to come down in the future," Wake wrote in an email.
Correlation was excellent between CAD and model dimensions (p < 0.001). Even so, measurements of the 3D-printed phantom were larger than the reference CAD measurements by an average of 0.04 mm. Tumor diameter measurements from the 2D image sets also correlated well with the 3D-printed models (< 0.001). Measurements on the 3D-printed model exceeded 2D measurements by an average of 0.76 mm (0.6% to 0.9%).
A Bland-Altman analysis suggested a slight systematic overestimation in size on both the 3D-printed measurement phantom and the 3D-printed kidney tumor models. The postoperative volume loss correlated with warm ischemia time but not with nephrometry score, a finding that will be further investigated in future studies.
Better planning for some surgeries
Whether or not 3D printing is indicated for every complex cancer will be explored in future studies, Wake said. A larger, prospective study is currently being implemented to determine the overall impact of the 3D-printed kidney models on preoperative planning.
"Our results showed that surgeons changed their planned decisions more for cases with larger volume loss and longer ischemia times than for other cases, which suggests that perhaps the 3D-printed models will only add value for certain complex cases," she said.