3D printing can be invaluable for training surgeons and can significantly shorten hip surgery times in patients with a common adolescent hip disorder, saving thousands in surgical costs, according to researchers from the University of California, San Diego (UCSD).
In a pilot study, a UCSD team explored the use of patient-specific 3D-printed models produced from CT scans to plan surgeries for slipped capital femoral epiphysis -- the most common hip disorder in adolescents ages 9 to 16. Surgeries that were preplanned using the 3D models required half the fluoroscopy time and were performed 45 minutes faster than surgeries that did not benefit from 3D models.
The shorter surgery times would save at least $2,700 per procedure, according to the team led by bioengineering doctoral student Jason Caffrey and medical student Lillia Cherkasskiy.
"Results suggest that 3D models may decrease surgical time and fluoroscopy time while allowing for similar deformity correction," the authors wrote in a paper published recently in the Journal of Children's Orthopaedics. "These models may be especially useful to overcome steep learning curves for complex procedures or in trainee education through mock surgical procedures."
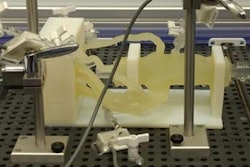
 UCSD surgeons found that 3D printing can shorten surgical fluoroscopy time in pediatric hip surgeries. Image courtesy of UCSD.
UCSD surgeons found that 3D printing can shorten surgical fluoroscopy time in pediatric hip surgeries. Image courtesy of UCSD.A challenging surgery
Slipped capital femoral epiphysis affects 11 in 100,000 children in the U.S. each year. The main goal of surgical intervention is to sculpt the femur back into its normal shape and restore hip function. However, this surgery -- called triplane proximal femoral osteotomy (TPFO) -- is challenging to perform because the bone and its growth plate are not directly visible; surgeons can't visualize in 3D how the growth plate is deformed, according to the authors.
Surgeons traditionally have planned the procedure by studying x-rays of the surgical site taken from different angles to determine where to perform the bone cuts. Fluoroscopy also is used periodically to help guide the procedure. But these methods are time-consuming and result in radiation exposure to the child, the authors noted (J Child Orthop, April 2017, Vol. 11:2, pp. 147-153).
The researchers sought to determine if 3D printing could decrease surgery and fluoroscopy time without sacrificing surgical accuracy. They performed a study involving 15 children scheduled to receive surgery for slipped capital femoral epiphysis. Of the 15, 10 children were treated by a single pediatric orthopedic surgeon, senior author Dr. Vidyadhar Upasani; five of these surgeries were planned with a 3D model, while five were not. The remaining five patients in the study were treated by two senior partners without the use of a model. The children all had similar body mass indexes.
3D models were created by first processing and converting pelvic CT studies to the stereolithography (STL) 3D printable format using the Mimics v17 software (Materialise). Additional processing and optimization steps were performed using the NetFabb Basic v5.2.1 software (NetFabb) and MeshMixer (AutoDesk) software applications.
The final STL file was then printed with acrylonitrile butadiene styrene on a TAZ 4 3D printer (Lulzbot). Each of the models was printed with a 20% honeycomb fill pattern with automatically generated supports; the honeycomb-like structure was selected due to its ability to mimic bone, according to the researchers. It took four to 10 hours for each model to be printed. Prior to performing the surgeries, the lead surgeon performed a mock surgery on the 3D model.
Faster surgeries
The 3D models led to sharp reductions in fluoroscopy and surgical time, the researchers found.
| Impact of 3D models on surgical and fluoroscopy time | |||
| Surgeries by 2 surgeons without 3D model | Surgeries by 1 surgeon without 3D model | Surgeries by 1 surgeon with 3D model | |
| Surgical time | 163.8 ± 43.8 min | 170.4 ± 76.4 min | 125.8 ± 25.4 min |
| Fluoroscopy time | 0.4 ± 0.2 min | 0.6 ± 0.4 min | 0.3 ± 0.3 min |
Due to the small sample size, however, the differences were not considered to be statistically significant. The time savings, though, would translate into at least $2,700 in savings per surgery, according to the authors. A 3D printer costs approximately $2,200, and each model can be printed for about $10.
Postoperative radiographic assessment found similar surgical outcomes among all patients. During follow-up, however, two of the five patients in the group operated on without a 3D model for presurgical planning later required surgical revision.
"These preliminary results suggest that 3D model use may decrease postoperative complications of TPFO, although further studies are needed to determine if this effect is statistically significant," the authors wrote.
Based on the study's results, the orthopedics department at Rady Children's Hospital has acquired its own 3D printer, according to senior author Upasani.
"I've seen how beneficial 3D models are," he said in a statement. "It's now hard to plan surgeries without them."