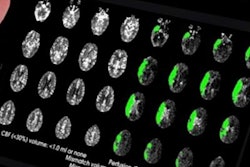
A 3D-printed brain perfusion phantom can be a useful tool for interventional radiologists, neurosurgeons, and neuroradiologists to practice performing mechanical thrombectomy for interventional treatment of stroke, according to a team from the University of Connecticut Health Center in Farmington, CT.
 David Brotman, clinical research assistant at Yale Cancer Center.
David Brotman, clinical research assistant at Yale Cancer Center.
"Currently, residents learn procedures on actual patients with ever-increasing responsibility for the procedure as their experience level increases," Yang told AuntMinnie.com. "I just feel that a training model allows one to get over the initial difficulty of being a novice when approaching a new task."
In addition to being useful for practicing mechanical thrombectomy, the 3D model could be helpful for understanding blood-flow dynamics -- especially in stroke or neurological tumors, said Brotman, now a clinical research assistant at Yale Cancer Center in New Haven, CT.
Stroke treatment
The standard of care for stroke treatment has traditionally been intravenous tissue plasminogen activator (tPA) to try to dissolve the clot blocking the blood flow. This method has limited success, however, and there is a narrow window of opportunity after the onset of symptoms before cells in parts of the brain deprived of blood begin to die and brain function is lost, Brotman said.
 Dr. Clifford Yang, cardiac radiologist at the University of Connecticut Health Center.
Dr. Clifford Yang, cardiac radiologist at the University of Connecticut Health Center.However, the U.S. Food and Drug Administration (FDA) recently approved the use of mechanical thrombectomy as a front-line treatment to reduce disability in patients experiencing acute ischemic stroke, he said.
"I saw this as an opportunity to develop a cheap training device that could mitigate stroke costs and provides hands-on thrombectomy-simulation experience to interventionists (interventional radiologists, neurosurgeons, and neuroradiologists) to improve comfort [levels], decrease variability, increase patient safety, and decrease overall procedure time, which are all critical to patient outcomes in stroke care," Brotman said.
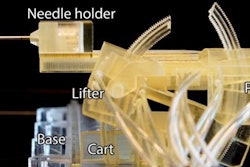
He spent a year developing the model, which is based on a patient's MRA and CTA studies. After deidentifying the DICOM image data, Brotman segmented the vascular structure using the 3D Slicer freeware software. Next, the segmented data were imported into the Meshmixer software (Autodesk) to combine the data; the MRA study covers the chest up to the bottom of the neck, while the CTA exam includes the neck to the top of the head.
The combined scans were then optimized and smoothed using the Netfabb additive manufacturing software (Autodesk). The finalized "mesh" was uploaded into the PreForm 3D printing software (Formlabs) to build support structures for printing on a Form 2 clear resin printer (Formlabs). The final phantom was then assembled, Brotman said.
Yang had some previous background in making medical models for medical imaging. He built a neuroperfusion training phantom with University of Connecticut biomedical engineer Mark Galiette several years ago, and he also created a cardiac training phantom that received a U.S. patent.
"That took me three years, but it was not a commercial success," Yang said. "It is too expensive to build."
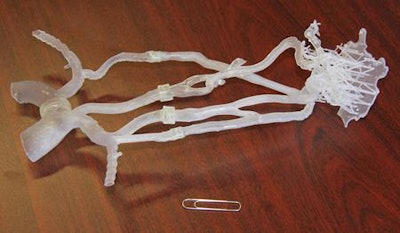 A 3D-printed brain perfusion phantom allows interventionists to practice mechanical thrombectomy procedures. All images courtesy of David Brotman and Dr. Clifford Yang.
A 3D-printed brain perfusion phantom allows interventionists to practice mechanical thrombectomy procedures. All images courtesy of David Brotman and Dr. Clifford Yang.Low cost
That's not the case for the 3D brain perfusion phantom, which could be printed for about $14, according to the researchers. Brotman has produced three vascular models for interventional vascular radiology training.
In a statement, Chief of Neurosurgery Dr. Ketan Bulsara cautioned, though, that individual anatomy varies too much for the model to be relied upon as the only training tool for learning mechanical thrombectomy. Bulsara also sees potential for 3D-printed models to visualize other conditions such as brain tumors; modeling the tumor in advance could personalize and enhance patient care by yielding significantly improved outcomes and reduced operating times, according to the university.
"We are currently working with Dr. Bulsara to make some custom models of his patients for preoperative neurosurgical planning," Yang said.
The 3D-printed phantom can also be seen as a form of disruptive technology, Brotman said. Trainee physicians could take the vascular simulator home to practice, for example. It could also be used in rural hospitals for training or even in third-world countries where simulation suites are not feasible.
"This represents a paradigm shift in the way medicine can be practiced," he said.
Yang and Brotman said they are willing to share the pattern used to create the model with physicians or researchers.