Creating 3D-printed hearts based on rotational angiograms is an effective alternative to using images from CT and MR, according to a recent study published in Pediatric Cardiology. These 3D-printed heart models can help physicians evaluate patients and prepare for upcoming procedures.
 Dr. Wilson King from Saint Louis University School of Medicine.
Dr. Wilson King from Saint Louis University School of Medicine.
"3D-printed models from rotational angiography are extremely precise when compared to the gold standard of biplane angiography," senior author Dr. Wilson King told AuntMinnie.com. "3D printing [from rotational angiography] is a powerful method to understand complex anatomy and improve patient care -- particularly from the standpoint of presurgical and preprocedural planning."
High spatial resolution
Interventional radiologists and surgeons have been taking advantage of the patient-specific quality of 3D-printed models to aid in preoperative planning. The vast majority of these models are based on CT or MR images of patients, which users slice and segment with 3D modeling software.
Besides CT and MRI, rotational angiography is a strong candidate for 3D printing due to its precision and the high spatial resolution of its 3D scans, according to the authors. The imaging modality is particularly well-suited for assessing hearts affected by congenital heart disease; rotational angiography makes it possible to visualize small, complex structures, and patients who are found to need therapeutic treatment are sent on to cardiac catheterization.
Considering the advantages of using rotational angiography to visualize the heart, King and colleagues set out to determine the feasibility and accuracy of producing 3D-printed hearts based on the 3D datasets of rotational angiograms. They collected the scans of five pediatric patients, each with a different heart disease, who underwent rotational angiography (Infinix-i, Canon Medical Systems) at Cardinal Glennon Children's Hospital in St. Louis between June and December of 2015. Next, they formatted the scans via 3D modeling software (Meshmixer, Autodesk) and printed 3D heart models with a PolyJet 3D printer (Objet Eden 260, Stratasys).
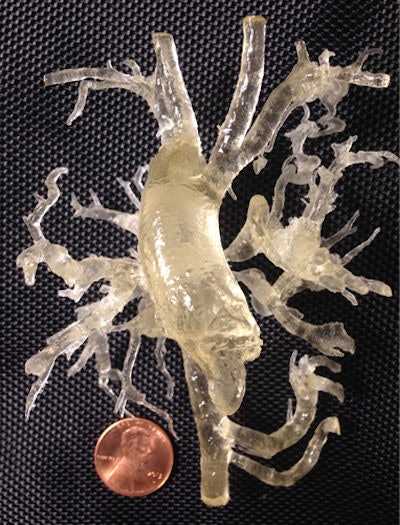 3D-printed model of a heart with tetralogy of Fallot and multiple aortopulmonary collaterals. Image courtesy of Dr. Wilson King.
3D-printed model of a heart with tetralogy of Fallot and multiple aortopulmonary collaterals. Image courtesy of Dr. Wilson King.Dimensions taken from five to 10 select locations on the resulting 3D-printed hearts displayed an "excellent" correlation with corresponding areas on the angiograms (R2 = 0.94, p < 0.05). There was no statistically significant difference between measurements of the scans and models (p = 0.14), as well as no significant variability between the two observers who completed the measurements.
Based on the group's estimations, each 3D-printed heart model took four to 12 hours to produce, at a relatively low cost of $75 to $200 per model.
'Uniquely suited'
In one of the more complicated cases, the researchers tested the usefulness of a patient's 3D-printed heart in a clinical setting. The 6-month-old had a rare condition, tetralogy of Fallot, that led to the development of multiple aortopulmonary collateral arteries and demanded an urgent and "extremely challenging" operation, according to King. Studying the patient's 3D-printed heart allowed the surgical team members to plan how they would dissect the otherwise elusive arteries and reconstruct them into a single pulmonary artery.
"We believed that rotational angiography was uniquely suited to comprehensively defining the aortopulmonary collateral anatomy due to both selectivity and resolution," he said. "Building a physical 3D-printed model at a 1:1 scale helped the surgeons understand the anatomy precisely and plan their surgical approach."
The success of the operation encouraged the group to prep more of the procedures for congenital heart disease using 3D-printed hearts based on rotational angiograms, and even refer to them intraoperatively, the authors noted. This would counter the chief limitation of the current study -- its low sample size.
In addition, they will continue to monitor the patients and "hope to expand this work to include [postsurgical] outcome studies in pediatric cardiovascular disease," King said.