Integrating 3D printing technology into presurgical planning for hip joint fracture repair can significantly reduce operating times and blood loss, compared with conventional methods, according to an article published online July 9 in Orthopaedics and Traumatology: Surgery and Research.
Repairing acetabular fractures, or breaks in the socket section of the ball-and-socket hip joint, has been a "challenging 'hotspot' for orthopedic surgeons ... [due to] the complexity of the local anatomy of the pelvis, diversity of fracture morphology, and inconvenience of bending plates," wrote corresponding author Xiaodong Guo and colleagues from Huazhong University of Science and Technology in China.
In addition, standard fracture repair involves shaping metal plates to fit the unique morphology of a patient's hip joint before surgery. Traditionally, clinicians have examined pelvic CT scans to help them contour the plates, but the limited visualization provided by the scans often requires the surgical team to reshape the plates during surgery -- increasing the risk of surgical complications, the researchers noted.
Exploring strategies to overcome these issues, Guo and colleagues investigated the potential advantages of using a combination of 3D printing technology and computer-assisted virtual simulations to bolster preoperative planning for acetabular fracture surgery.
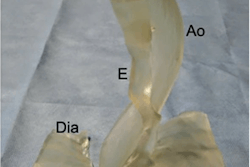
They began by obtaining the pelvic CT scans of 52 patients who required fracture repair. For roughly half of the patients, they segmented the CT scans and converted them into virtual 3D models using computer software (Mimics 16.0, Materialise). Then they imported the data as stereolithography (STL) files into 3D printing software (Cura, Ultimaker) for production. It took approximately 12 hours to create each 3D-printed model.
Before initiating surgery on the first patient cohort (roughly half the participants), the researchers used the resulting individually tailored 3D-printed hip models to contour the reconstruction plates. They also practiced the procedure via a computer-assisted virtual simulation. The other half of the patient cohort received presurgical planning for fracture repair with the conventional technique.
After performing the surgeries, the team found that the 3D printing patient cohort had statistically significant reductions in blood loss and operating time, compared with the patients who received the standard surgical treatment. Furthermore, the 3D printing group received slightly higher scores than the other patients in regards to the quality of the repair and postoperative hip function based on two commonly used surgery-rating scales, though the differences were not statistically significant.
| 3D printing vs. conventional method for hip joint fracture repair | ||
| Conventional method | 3D printing | |
| Intraoperative blood loss | 834 mL | 696 mL |
| Operating time | 3 hours, 7 minutes | 2 hours, 38 minutes |
The conventional method also required surgeons to recontour the plates during the operation to fit individual patients more precisely -- increasing overall surgery time by an average of 18.8 additional minutes per case. In contrast, having access to patient-specific 3D-printed hip models enabled the surgical team to contour the plates accurately during presurgical planning instead of performing this step intraoperatively.
One of the drawbacks of applying 3D printing is the increase in production costs, which amounted to approximately 500 yuan ($73 U.S.) for a single 3D-printed hip model. However, the 3D printing method cut roughly 30 minutes of operating time for each patient, and the savings in surgical costs generated by this reduction far surpassed the price of a single model, the authors noted.
"3D printing technology is a highly clinically relevant technology, especially in the treatment of complex acetabular fractures," they wrote. "A patient-specific precontoured plate can indeed reduce the operative time and blood loss to improve the accuracy and preciseness of surgical implant preparation in a real sense."