Quantitative analysis of texture patterns on CT exams in interstitial lung disease patients can yield better survival predictions than a radiologist's classification of usual interstitial pneumonia (UIP) versus non-UIP, according to research presented at last week's virtual ECR.
Researchers from the University of Pennsylvania developed a texture-based image classification model for high-resolution CT that substantially outperformed expert radiologist classifications of UIP versus non-UIP in predicting survival in a study involving 40 interstitial lung disease patients.
"These models, by capturing latent quantitative CT-derived lung parenchymal texture features not explicitly accounted for in clinical diagnostic labels such as UIP versus non-UIP, may provide more accurate prognostication, ultimately contributing to more effective patient management and possibly improving long-term outcomes," said presenter Dr. Eduardo Mortani Barbosa Jr.
Fibrosing interstitial lung diseases require considerable expertise to diagnose and manage, and confident diagnosis may be elusive even when expert multidisciplinary discussion teams review the case, according to Barbosa.
Usual interstitial pneumonia tends to have a worse prognosis than non-UIP patterns of interstitial lung disease. The researchers hypothesized, however, that a texture-based model of utilizing high-resolution quantitative CT imaging features could analyze the data in a way that would enable better prediction of survival in these patients compared with the current clinical standard of UIP versus non-UIP diagnostic labels by radiologists.
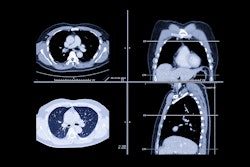
UIP has a typical pattern on CT consisting of reticulation and honeycombing with a peripheral and basilar-predominant distribution, he said. On the other hand, non-UIP patterns of interstitial lung diseases such as chronic hypersensitivity pneumonitis or non-specific interstitial pneumonia also have distinct CT features. Barbosa said.
In a retrospective study, the researchers collected 40 patients with interstitial lung disease, including 20 with a UIP pattern and 20 with a non-UIP pattern on CT. These diagnoses were made in consensus by two expert radiologists.
Each patient received high-resolution CT exams, with 1-mm contiguous volumetric axial images obtained in inspiration. The researchers also noted clinical variables for each patient, including age, gender, smoking history, and emphysema. The patients were followed up for seven years, and outcomes included time to death or time to lung transplantation.
Using a 3D k-means clustering approach, a texture-based model identified two distinct clusters of texture metrics from analysis of 26 higher-ordered image texture features on the CT exams. These texture clusters correlated with worse or better survival rates.
To compare how well the radiologist diagnoses and the texture model's results correlated with patient survival, the researchers generated Kaplan-Meier curves for the expert diagnostic labels of non-UIP versus UIP pattern on CT, as well as for two specific texture clusters identified by the model that were associated with either worse or better survival rates.
"UIP versus non-UIP expert labels did not allow us to partition the cohort into distinct survival groups; the p-value is not statistically significant," he said. "Whereas the texture-based model does allow the partition of the cohort into two distinct clusters of different survival."
In future directions, the researchers plan to validate their texture-based quantitative CT predictive models on a much larger cohort of over 500 interstitial lung disease patients, Barbosa said.