MRI volumetric analysis based on a deep-learning segmentation algorithm helps assess intracranial and white-matter volumes in Parkinson's disease patients, according to research presented November 26 at the recent RSNA meeting.
Parkinson's disease causes structural changes in subcortical brain volumes, and it's important to track these, noted a team led by Nikhil Gupta, MD, of Tirath Ram Shah Hospital in Delhi, India. Gupta's group assessed the ability of an MRI technique -- volumetric analysis based on a deep-learning segmentation -- to visualize volumetric abnormalities in Parkinson's patients compared to healthy controls.
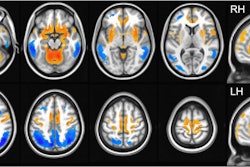
The team performed a study that included 100 patients with Parkinson's and 100 without the disease who underwent 3D T1-weighted MR imaging. The investigators then used InMed Prognostics' euroShield deep-learning algorithm to segment and calculate intracranial, white-matter, and gray-matter volumes and the volume of deep gray-matter structures.
There were no significant differences in gray-matter or deep gray-matter volumes between the two groups, but intracranial volume was significantly higher in Parkinson's patients compared with controls (p = 0.01) -- a finding that was unique to the men in the study (p = 0.002). Gupta and colleagues also found that white-matter volume was significantly lower in Parkinson's patients compared with controls (p = 0.03), which was again only significant among men (p = 0.02).
"As intracranial volume can be significantly higher in Parkinson's disease patients compared to controls it is key to accurately measure and consider intracranial volume in volumetric analysis of [these individuals]," they concluded.
In a related presentation delivered during the same session, presenter Chae Jung Park, MD, of Yonsei University College of Medicine in Seoul, South Korea, shared results from a study that found that choroid plexus (i.e., the network of blood vessels in the brain) volume could serve as a biomarker for tracking baseline and longitudinal motor disabilities in patients with Parkinson's.
The study assessed 322 patients with early-stage Parkinson's disease who underwent dopamine transporter scanning and high-resolution 3-tesla T1-weighted structural MRI. Park and colleagues automatically segmented the choroid plexus volume of each patient and assessed the relationship between choroid plexus volume and baseline Unified Parkinson’s Disease Rating Scale Part III (UPDRS-III) scores (which were adjusted for age at symptom onset, sex, disease duration, body mass index, and white matter high signal intensity volumes).
The investigators found that larger choroid plexus volumes were associated with the future development of poor longitudinal motor outcomes, particularly freezing-of-gait (hazard ratio, 1.5, with 1 as reference).
"[Our study suggests] that a choroid plexus volume is associated with parkinsonian motor deficits at initial assessment, as well as poor outcomes with respect to the progression of motor disabilities during the follow-up," Park concluded. "The choroid plexus volume, which can be easily and automatically obtained from MRI, has the potential to serve as a biomarker for baseline and longitudinal motor disabilities in Parkinson's disease patients."