When it comes to the advantages of percutaneous breast biopsy over surgical excision, breast imaging experts are in the know -- image-guided biopsy can be performed quickly using local anesthesia, ensures better patient compliance, and is cost-effective. MRI-guided biopsy in particular can offer a procedure time of less than an hour. Unfortunately, this good news hasn't necessarily made its way to the offices of referring physicians.
Two recent studies took a closer look at current techniques and trends in breast biopsy. First, Dr. Laura Lieberman and colleagues report on their clinical experience with an MRI-guided 9-gauge vacuum-assisted procedure. In a second study, Dr. Elizabeth Lazarus and co-authors decipher the effect of physician specialty and practice type on image-guided breast biopsy.
'Fast and safe alternative' to surgical biopsy
Lieberman's study population consisted of 106 women scheduled for biopsy at Memorial Sloan-Kettering Cancer Center in New York City. These women had 112 MRI-detected lesions that were deemed suspicious or highly suggestive of malignancy.
"Each MRI lesion was described ... before biopsy as mass, nonmass, or focus of enhancement, and further categorized on (BI-RADS) breast lexicon," they explained. Out of the 112 lesions, 101 were solitary, with the majority presenting as masses, and with a median size of 1.0 cm (American Journal of Roentgenology, July 2005, Vol. 185:1, pp. 183-193).
Biopsies were performed by nine breast imagers using a 9-gauge, MRI-compatible, vacuum-assisted device (Automated Tissue Excision and Collection, Suros Surgical Systems, Indianapolis). Patients were offered 1.0 mg of oral lorazepam before being positioned in a prone manner in a 1.5-tesla scanner with a dedicated breast surface coil. The authors described their technique in a previous article (AJR, November 2003, Vol. 181:5, pp. 1283-1293).
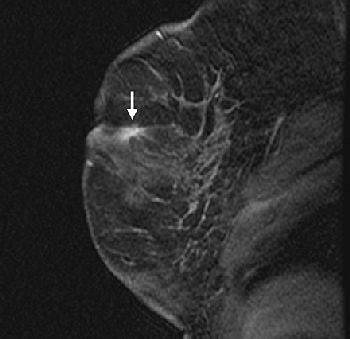 |
| Fifty-four-year-old woman with history of left breast cancer with normal mammogram and no palpable lumps, in whom MRI detected speculated right breast mass with no sonographic correlate. Sagittal fat-suppressed T1-weighted, contrast-enhanced scout image from MRI-guided biopsy shows 0.9 cm mass with speculated borders, irregular shape, and heterogeneous enhancement in right retroareolar region (arrow). |
According to the results, MRI-guided biopsy was attempted in 98 lesions with tissue acquisition achieved in 95. The clip was successfully deployed in 86 cases, and the median number of specimens obtained was 12. The median performance time for MRI-guided biopsy was 33 minutes for a single lesion.
"Most of the time ... is due to imaging, which generally includes a precontrast three-plane MRI localizer and a minimum of four contrast-enhanced, fat-suppressed sagittal T1-weighted MRI scans," the authors stated.
In those 95 lesions, histology was benign and concordant with imaging in 55% of the cases. Cancer was detected in 25%, with the majority being ductal carcinoma in-situ. Eleven percent were labeled as high-risk lesions.
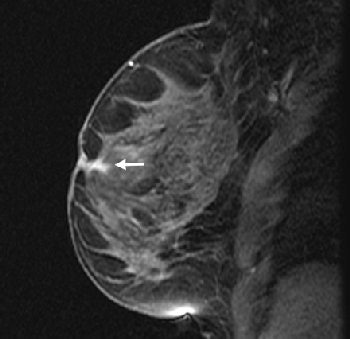 |
| Same patient as above. Sagittal fat-suppressed T1-weighted, contrast-enhanced MRI on date of MRI-guided needle localization shows persistence of right retroareolar speculated mass (arrow). MRI-guided needle localization yielded 0.5 cm infiltration ductal carcinoma and ductal carcinoma in-situ. Liberman L, Bracero N, Morris E, Thornton C, Dershaw DD, "MRI-Guided 9-Gauge Vacuum-Assisted Breast Biopsy: Initial Clinical Experience" (AJR 2005;185:183-193). |
Histology-imaging discordance occurred in 9% of the cases. Subsequent surgical biopsy showed cancer in four out of the nine latter cases. The MRI target was completely excised in 29% of the cases. There were six complications, including instances in which the biopsy probe pierced the skin on the far side of the breast. These were treated and resolved, the authors stated. Finally, a diagnostic surgical biopsy was spared in 78% of the 95 lesions in which tissue was acquired.
At a median follow-up of seven months, there were 31 MRI exams and no evidence of cancer was identified in 94% of the cases. The authors reported a 97% technical success rate with MRI-guided biopsy with a 25% positive predictive value.
Future research in this area should focus on optimal timing for follow-up MRI after biopsy, as well as whether specimen imaging of MRI lesions would be prudent, the researchers concluded.
Self-referral rears its ugly head
If image-guided breast biopsy, either with MRI, ultrasound, or stereotactic guidance, is so beneficial, why don't more nonimaging specialists take notice of it? The answer to this question may be as benign as a lack of information or as insidious as an excess of self-interest.
"The factors that influence a physician to recommend excisional biopsy over image-guided biopsy are often unclear," wrote Lazarus and co-author Dr. Martha Mainiero, who are both from the diagnostic imaging department at Brown Medical School in Providence, RI. A third co-author, Ilana Gareen, Ph.D., is from the departments of biomedical ethics and community health at Brown University, also in Providence (Journal of the American College of Radiology, June 2005, Vol. 2:6, pp. 488-493).
The goal of their retrospective study was to determine whether physician specialty or practice type influenced biopsy recommendations. The data for this research was collected from five outpatient imaging centers where multimodality breast imaging is performed but biopsies are not, and a hospital where percutaneous image-guided biopsies are done. The covariates for the analysis included physician specialty, such as surgeon or ob/gyn, as well as patient age and lesion palpability.
During the year 2000, 39,528 mammograms and 4,532 ultrasound exams were done at all six facilities. From these exams, 831 BI-RADS 4 and 5 reports were generated with 1% of these cases specifically recommended for excisional biopsy. Eighty-eight percent underwent either ultrasound-guided core-needle biopsy or stereotactic vacuum-assisted biopsy. The remaining patients were excluded from the analysis because either there was no follow-up or they declined to undergo biopsy.
The results showed that the specialty of the referring physician impacted the type of biopsy procedure. Patients referred by surgeons versus nonsurgeons were more likely to undergo surgical biopsy. The authors offered possible reasons why.
"Our study suggests that physicians who can self-refer for excisional biopsy are more likely to recommend (it).... Surgeons may have a direct monetary incentive to perform excisional biopsy rather than to refer the patient for imaged-guided biopsy," they wrote. Other reasons include the age of the surgeon -- older doctors may not be as familiar with image-guided biopsy, which really emerged in the 1990s -- or a belief that surgery is the better procedure because it completely removes the lesion.
Patients referred by an ob/gyn or an internist were more likely to undergo imaged-guided biopsy. These doctors rarely perform biopsies of any kind, eliminating the conflict of interest that confronts surgeons, the authors stated.
Other factors that weighed in on the side of surgical biopsy were BI-RADS category 4 and 5 lesions and palpable lesions. Patient age was not related to biopsy type.
While imaging advocates continue to grapple with the self-referral issue, breast imagers should consider educating the public, as well as their peers, as to the benefits of image-guided biopsy, the authors stated. This can be done on a broader level with health education campaigns, or on an individual level, such as a meeting with the radiologist, referring doctor, and patient at the time of diagnosis to discuss biopsy options.
By Shalmali Pal
AuntMinnie.com staff writer
July 29, 2005
Related Reading
Breast rads believe malpractice fears prompt more recalls, June 28, 2005
PPV alone not enough to assess mammo screening program, May 23, 2005
Breast MRI OK immediately following biopsy, March 9, 2005
Breast biopsy costs big bucks, but so does cancer screening, January 19, 2005
Copyright © 2005 AuntMinnie.com