Bullet trains have always fascinated me. It's as if they were visitors from a not-so-remote future that accidentally slipped back a decade to be with us here and now. It seems we can't even watch the nightly news without seeing other examples of the future that showed up early -- from absurd dancing robots to amazing telerobotic surgery. A harbinger of healthcare's future that seems to have come early is intraoperative imaging.
In a recent article ("Interventional MRI: Out of the scanning suite and into the OR"), we described how MRI, developed strictly as a diagnostic tool, has expanded beyond its original boundaries, and has become an integral part of interventional procedures. This earlier article addressed how existing diagnostic suites can be retooled and retasked to support minor interventional procedures. The far other end of the spectrum, the part that makes us feel as if we're gazing into the near future, is a complete rethinking of how MRI is used and the value of providing diagnostic imaging in the operating suite.
Having seen Technicolor-rainbow images of neurological scans, it may be surprising that the actual gray matter inside a person's head is remarkably indistinct. A tumorous mass may glow phosphorescent orange on the MRI console, but it's just gray tissue, indistinguishable from the surrounding gray tissue, when your head is opened up in the operating room. It is for this reason that it has been extremely difficult for neurological surgeons to balance aggressive surgical treatments against the potential for damaging crucial healthy areas of a patient's brain. Too often residual portions of a tumor are revealed in a postoperative scan, necessitating follow-up surgeries.
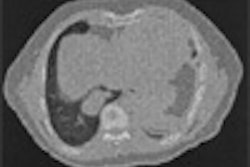
But what if you could receive an MRI while you're still in the operating suite? What if surgeons could verify that they'd removed the entire tumor while you were still on the table, removing the potential need for follow-up surgeries? What if the diagnostic feedback was instantaneous and an integral part of the interventional procedure? This has been done for years with C-arms, but just now is gaining traction with CT and MRI.
For the moment we can't put conventional MR or CT technology on an arm within the OR. The gantries are too big, and the safety concerns with both radiation exposure and magnetic field effects make siting the devices in the OR difficult. But imaging rooms interconnected with the surgical theater bring the elements of a diagnostic scan, procedure, and postoperative scan into such an arrangement that all can be done as part of a single procedure. This configuration allows patients to be taken to an adjacent next-door sterile environment for imaging while still sedated for a surgical procedure.
This service hybridization, erasing the lines of separation between diagnostic and interventional services, is being refined in the Boston area by the Center for Integration of Medicine and Innovative Technology (CIMIT), a consortium of healthcare providers and educators, under the name Advanced Multimodality Image-Guided Operating Room (AMIGO). The AMIGO principle is to gather key diagnostic modalities in a suite of interconnected rooms surrounding an OR to allow for testing and evaluating which diagnostic tools have the greatest utility in the surgical environment. Some modalities, such as C-arms and ultrasound will undoubtedly have a place in the OR, while conventional CT and MRI will be located in interconnected adjacent rooms. The surgical patient will be able to be transported into an adjacent room for scans and can be returned to the OR for follow-up as indicated by the intraoperative scan.
And if Mohammed can't go to the mountain, let the mountain come to him.
A spin-off from Canada's Institute for Biodiagnostics is the IMRIS (Winnipeg, Manitoba) MRI system, which mounts a 1.5-tesla MRI to an overhead track instead of the floor. This allows the MRI to travel from a storage area, or even an adjacent diagnostic suite, into an operating room.
By aligning the specially designed surgical table with the IMRIS track, the MRI can be brought into the surgical suite and slide right over (around) the patient on the table. This system allows for surgical and imaging procedures to intersperse without ever having to move the patient. The fact that the MRI can exit the room also means that the surgeons can use standard surgical tools and devices. Only those devices (such as anesthesia machines) that need to remain at the patient's side need to be MR-safe or MR-compatible. All other nonsafe tools and devices can simply be removed from the OR for the duration of the scan.
Clearly there are a number of hurdles with regard to intraoperative imaging, from potential AMIGO modality conflicts to the ever-present suite safety issues with MRI. It may not be easily accomplished, but the dissolution of the artificial border between diagnostic and interventional services will produce better healthcare. The programs, protocols, and even the suites needed to support AMIGO and IMRIS may be equally complicated, but I expect that if bullet trains were easy to build, there'd be one outside my office.
By Tobias Gilk
AuntMinnie.com contributing writer
August 31, 2005
Reprinted from www.mri-planning.com by permission of the authors. If you would like more information on any aspect of MR facility design or safety, please contact Robert Junk or Tobias Gilk at Jünk Architects.
Related Reading
When good vibrations go bad -- an MRI full of sound and fury, August 2, 2005
Did the MRI community learn from the Colombini tragedy? July 28, 2005
Interventional MRI: Out of the scanning suite and into the OR, July 8, 2005
MR safety versus the bottom line: Why safety pays, June 16, 2005
Construction planning outside the MRI suite, June 9, 2005
Copyright © 2005 Jünk Architects, PC