VIENNA - Some urologists continue to persist with the old methods of prostate biopsy and tumor detection, despite the benefits of MRI in visualizing the most aggressive parts of prostate tumor, but the situation is changing fast, according to Dr. Jelle Barentsz, PhD, from the department of diagnostic radiology at University Hospital Nijmegen in the Netherlands.
The reasons behind this apparent resistance in some quarters are unclear, but it seems to be due to a combination of skepticism, turf protection, and financial aspects. The chief arguments put up by urologists against embracing MRI-guided biopsies in the first instance tend to be cost, lack of expertise with certified standards for radiologists, and lack of large prospective randomized controlled trials.
 The day will come when prostate cancer patients are treated on an outpatient basis only, according to Dr. Jelle Barentsz, PhD.
The day will come when prostate cancer patients are treated on an outpatient basis only, according to Dr. Jelle Barentsz, PhD.
This stance is refuted by Barentsz, who claims that, just like learning to drive, urologists need to learn the technique from experts, gain experience and then be tested for their surgical expertise. He considers that radiologists need to have read a minimum of 200 examinations under supervision, with good standards for quality control at a central reference center, and they must adhere to guidelines that have been developed by the European Society of Urogenital Radiology. Although these guidelines are not yet mandatory, Barentsz and his colleagues are collaborating with the American College of Radiology to further this process.
ECR delegates attending this afternoon's prostate session, which forms part of the daylong Mini Course on oncologic imaging, will learn about how to navigate their way through some of the blurring of boundaries in this specialist area, and can hear the latest advances in MR-guided prostate biopsy. Other speakers throughout the day will discuss lung, colon, kidney, liver, pancreatic, and ovarian cancers, and there will be a discussion of musculoskeletal neoplasms and issues around chemo- and radiation-induced toxicity.
"Transrectal ultrasound (TRUS) biopsy has a true underestimation of 46%, whereas some studies show that the underestimation rate with MRI is only 5%," said Barentsz, who conceded that further large prospective trials are required to confirm this, but the studies are under way.
Barentsz is very involved with patient groups. He thinks that patients are becoming more aware and empowered, and he notes that many patients are now discussing the MR-guided ultrasound biopsy ("needle biopsy") procedure and are asking about alternatives.
"If the patient has a negative TRUS biopsy and the prostate-specific antigen (PSA) is still rising, this is an absolute indication to do an MRI. It may be that the urologist has missed the tumor, and this occurs in between 46% and 50% of cases; however, the MR-guided biopsy will locate the lesion," he stated. "The other clear indication for MRI is when the patient requires treatment and needs a staging MRI, to visualize the prostate and see whether the tumor is at the aggressive or intermediate stage."
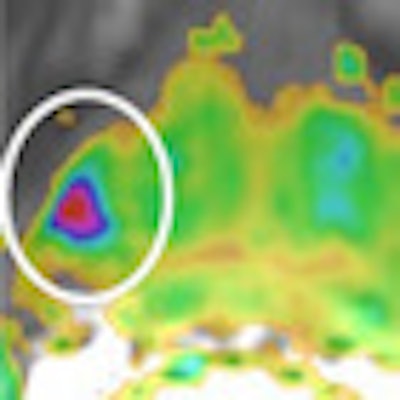
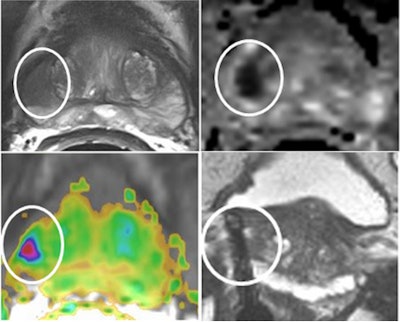 A 69-year-old patient with a low-grade (Gleason 3+3) prostate cancer (1/10 cores positive, < 5%) confirmed by transrectal ultrasound biopsy. Therefore, the patient was a candidate for active surveillance. Top left: T2-weighted MRI shows low-signal lesion (circle) in right peripheral zone. Top right: ADC map shows restriction is this area (ADC value: 650), and bright area on high b value (1400) diffusion-weighted image. Bottom left: Dynamic contrast-enhanced MRI shows focal unilateral area with curve type 3. Prostate imaging reporting and data system (PI-RADS) classification for significant cancer: 5-5-5, final score 5. This fits an aggressive tumor. Bottom right: MR-guided biopsy shows lesion (circle); needle = white line, showed 2/2 cores each 80% Gleason 4+3 prostate cancer. Due to this MRI examination, this patient's prospects have improved, and he will now have a prostatectomy. Images courtesy of Dr. Jelle Barentsz, PhD.
A 69-year-old patient with a low-grade (Gleason 3+3) prostate cancer (1/10 cores positive, < 5%) confirmed by transrectal ultrasound biopsy. Therefore, the patient was a candidate for active surveillance. Top left: T2-weighted MRI shows low-signal lesion (circle) in right peripheral zone. Top right: ADC map shows restriction is this area (ADC value: 650), and bright area on high b value (1400) diffusion-weighted image. Bottom left: Dynamic contrast-enhanced MRI shows focal unilateral area with curve type 3. Prostate imaging reporting and data system (PI-RADS) classification for significant cancer: 5-5-5, final score 5. This fits an aggressive tumor. Bottom right: MR-guided biopsy shows lesion (circle); needle = white line, showed 2/2 cores each 80% Gleason 4+3 prostate cancer. Due to this MRI examination, this patient's prospects have improved, and he will now have a prostatectomy. Images courtesy of Dr. Jelle Barentsz, PhD.Compared with pelvic phased-array coils, the chief benefits of using endorectal coils are the better higher signal-to-noise ratio and the detection of minimal capsular penetration. With a 1.5-tesla MR machine, the endorectal coil should be used, although the question as to whether an endorectal coil should be used with a higher field strength system is still under investigation. Barentsz also noted the high cost and patient discomfort as disadvantages of the endorectal coil. Three-tesla machines offer the advantage of higher throughput of patients, and this increases their cost-effectiveness.
A multiparametric approach promises improved detection and characterization of prostate cancer. He thinks the way forward is T2-weighted diffusion and dynamic imaging. Future perspectives in prostate cancer imaging look set to be interesting, and he welcomes the day when all patients will have an MRI examination before they have a biopsy. Contrast agents such as iron oxide particles (small nanoparticles that travel to the lymph nodes) promise to assist in the detection of small (2 mm) lymph nodes. Barentsz hopes for more precise diagnosis of prostate cancer, which he believes will be achieved with the use of MR-ultrasound fusion and minimally invasive therapy by treating localized tumors with high-intensity focused ultrasound under MR guidance.
Looking even further into the future of prostate treatment, he envisages the day when patients will be treated on an outpatient basis only; e.g., they will arrive in the morning for an MR-guided biopsy and histological confirmation, have a prostate tumor evacuated/treated via MR-guided cryo/needles, and leave the hospital the same day. The future is already here, he concluded.
Originally published in ECR Today on 8 March 2013.
Copyright © 2013 European Society of Radiology