German researchers have developed a 3D printing technique for producing realistic CT phantoms that radiologists were able to apply to the simulation of a CT-guided pain therapy procedure, according to results presented at ECR 2018.
In research presented in two separate sessions, investigators from Charité Universitätsmedizin in Berlin used a standard desktop printer containing radiopaque ink to print the CT scans of a patient onto regular sheets of paper; they then formed this stack of paper into a 3D-printed model using a 3D printer. After implementing a grayscale correction to the prints, they found that CT scans of the resulting 3D-printed model had a near-perfect correlation to the original CT scans of the patient.
"Radiopaque 3D printing allows [clinicians] to create detailed patient phantoms, which can be used for CT testing in a clinical setting," presenter Dr. Paul Jahnke told session attendees. "Radiopaque 3D-printed anthropomorphic phantoms allow highly realistic simulation of CT-guided procedures and can be used for training, procedure optimization, and development of interventional techniques."
Realistic anthropomorphic phantoms
Conducting research and practicing procedures on CT phantoms is advantageous because it safely allows for an unlimited number of scans with consistent testing conditions, according to Jahnke. But most phantoms have a narrow range of Hounsfield units and often do not adequately replicate the distinct characteristics of human anatomy upon radiological imaging.
Various groups have recently resorted to fabricating patient-specific phantoms through 3D printing. Following this trend, Jahnke and colleagues set out to use 3D printing to create phantoms that not only appeared lifelike externally but also replicated anatomic details on CT scans as well.
To achieve this objective, they acquired CT scans of an individual's abdomen and printed 10 identical scans of 10 consecutive CT sections (with 1-mm section thickness) on plain paper using a computer printer (HP Deskjet 6940, Hewlett-Packard). The printer was filled with a radiopaque ink containing 600 mg of potassium iodide per mL of ink. Next, they calibrated the grayscale of this 3D stack to match its Hounsfield units to those of the original patient CT scans. Applying this grayscale correction technique led to a correlation of more than 99% between CT scans of their 3D model and the original scans.
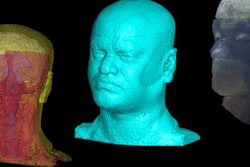
To convert the 3D stack into a 3D-printed model, they used a commercial 3D printer to automatically pull the printed sheets of paper from the paper tray as well as cut and glue the sheets into the shape visible in the scans. Applying this technique, they were able to create realistic 3D-printed phantoms of various body parts, including the hand, head, and neck, and test various CT protocols and parameters by examining scans of these phantoms.
"We were now able to use these phantoms for systematic investigation of CT parameters," Jahnke said. "You can take a phantom, put it in the CT [machine] once, and then you do all the acquisitions that you want, with all the combinations of imaging parameters that you like, and you get results or images as if you had tested on a real patient."
Strong similarity
Following parameter testing, the group set out to determine the viability of incorporating 3D-printed CT phantoms into the simulation of CT-guided procedures.
"Visual guidance is a key component of CT-guided procedures, and practice objects should match the patient anatomy as closely as possible," Jahnke said.
For the simulation, 10 interventional radiologists performed CT-guided periradicular infiltration on a radiopaque 3D-printed phantom of the abdomen that the researchers attached to a mannequin and covered with sterilized sheets to make the simulation seem as realistic as possible.
Among the 10 interventional radiologists, nine agreed or strongly agreed that the representation of the interior anatomic structures of the phantom, needle navigation, and overall course of the simulation were realistic. All 10 agreed or strongly agreed that the 3D-printed phantom was suitable for resident training for this particular procedure.
What's more, there was a strong similarity between the quantitative outcomes of these simulations on 3D-printed phantoms and those of 50 real clinical procedures on patients previously completed by these interventional radiologists: There were no statistically significant differences in the total number of scans acquired, procedural time, needle tip visibility, and needle corrections (p > 0.05).
"Indeed, visual guidance is a key aspect of CT-guided procedures and realistic phantoms can be valuable tools for training and simulation of CT-guided procedures," he said. "Other major fields of application [of radiopaque 3D printing] are in ... patient dose and radiation therapy and in training of clinical staff."