Augmented reality (AR) technology shows potential for improving the speed and safety of liver tumor ablation procedures, according to research presented during a virtual session of the Society of Interventional Radiology's (SIR) annual scientific meeting.
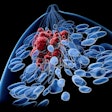
In an initial pilot study, a team of researchers led by Dr. Gaurav Gadodia, a radiology resident at Cleveland Clinic, tested the use of holograms to provide a 3D holographic view inside a patient's body and guide liver tumor ablation. Yielding similar results to standard ultrasound guidance, the AR technology enabled interventional radiologists to accurately burn away the tumors while navigating to avoid organs and other critical structures.
"Converting traditional two-dimensional imaging into three-dimensional holograms which we can then utilize for guidance using augmented reality helps us to better view a patient's internal structures as we navigate our way to the point of treatment," said Gadodia in a statement. "While conventional imaging like ultrasound and CT is safe, effective, and remains the gold-standard of care, augmented reality potentially improves the visualization of the tumor and surrounding structures, increasing the speed of localization and improving the treating-physician's confidence."
The technology involves the use of multiphase CT to record coordinate markers placed on a patient's body. After this imaging data is added to a software application for segmentation of the tumor and nearby structures within the marked coordinate space, the information is fed into a proprietary augmented reality application that utilizes Microsoft's HoloLens headset. A segmented hologram of the patient's imaged anatomy -- registered to the coordinate markers to ensure accurate location -- is then projected directly onto the patient.
With the use of electromagnetic tracking, instruments such as the ablation probe can be visualized in the augmented reality space during the procedure, enabling holographic intraprocedural guidance, according to the researchers. Interventional radiologists can then utilize the holographic images and the tracked tools to quickly find the tumor in the patient's liver, check for optimal targeting of the tumor by the ablation probe, and avoid key structures, they noted.
The researchers evaluated the technology in five patients who were to receive microwave ablation of their liver tumors. In all five cases, intraprocedural holographic guidance was in agreement with the standard ultrasound-based guidance.
In anecdotal observations, the authors found that the speed of tumor localization was faster with holographic guidance. In addition, their confidence in optimal ablation and critical structure avoidance was improved over standard imaging guidance. They said they are attempting to further quantify these findings as more patients are enrolled in this study.
Interventional radiologists also believe the technology could have value for planning purposes and to improve patient engagement and understanding of their condition and treatment.
The researchers said they are continuing to test the technology for guiding ablations in the abdominal area, and they plan to expand to other types of procedures and in other areas of the body.