A nomogram can help predict relapse in patients with prostate cancer who undergo prostate-specific membrane antigen (PSMA)-PET-guided radiotherapy after prostatectomy, according to a study published May 23 in JAMA Network Open.
A group led by Dr. Constantinos Zamboglou, PhD, of the University of Freiburg in Germany, developed the nomogram using data from 1,029 patients. The model performed well, and it could be used to help identify patients early who could benefit from further treatment, the authors suggested.
"No predictive tools for biochemical relapse estimation among this patient population currently exist," the group wrote.
Up to 50% of patients with prostate cancer develop a biochemical relapse within the first five years after primary radical prostatectomy, with guidelines recommending early salvage radiotherapy (sRT) of the prostate bed in these patients, with or without androgen deprivation therapy (ADT).
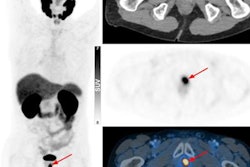
Predictive nomograms are widely used to provide individualized estimates of biochemical relapse after sRT, and with PSMA-PET being used increasingly to guide sRT after radical prostatectomy, the group aimed to develop a model that can predict relapse in these cases.
The researchers gathered data on 1,029 patients with prostate cancer treated between July 2013 and June 2020 at 11 centers from five countries. All patients had detectable post-radical prostatectomy prostate-specific antigen (PSA) levels after sRT, with relapse defined as a PSA nadir of 0.2 ng/mL. The median follow-up for all patients was 32 months.
An analysis revealed that the following factors in the patients were strongly associated with relapse hazard ratios: pre-sRT PSA level, International Society of Urological Pathology grade in surgery specimen, stage of the disease (pT stage), surgical margins, ADT use, sRT radiation dose, and nodal recurrence detected on PSMA-PET scans.
Based on these metrics, they created the monogram and then tested it in an internal validation set (n = 271), and external outlier validation set (n = 50). The model estimated freedom from biochemical recurrence with a score of 0.72 (area under the receiver operating characteristic curve) in the internal validation cohort and a score of 0.67 in the external validation cohort.
"This cohort study of patients with prostate cancer presents an internally and externally validated nomogram that estimated individual patient outcomes after PSMA-PET-guided sRT," the researchers wrote.
Ultimately, predictive nomograms can help physicians and patients make decisions about sRT. Although PSMA-PET is increasingly used in this disease stage, all currently available nomograms were created before the implementation of PSMA-PET for sRT guidance, the authors noted.
"To our knowledge, this multicenter study developed the first nomogram to predict [freedom from biochemical recurrence] for PSMA-PET-based sRT in recurrent prostate cancer," the group concluded.