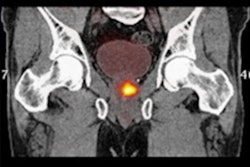
Negative prostate-specific antigen (PSMA) PET scans can be used to avoid unnecessary pelvic lymph node dissection in certain prostate cancer patients undergoing radical prostatectomies, according to a recent study.
While pelvic lymph node dissection (PLND) is the gold standard of nodal staging in men at intermediate risk, it carries its own risks and has no known benefit in this patient subgroup, noted a team of researchers from Hamburg, Germany.
“New promising imaging modalities such as PSMA-PET might help to select the right patients for PLND during [radical prostatectomy],” wrote lead authors Reha-Baris Incesu, MD, and Felix Preisser, MD, of the Martini-Klinik Prostate Cancer Center. The study was published January 6 in Prostate Cancer and Prostatic Diseases.
Studies have shown that a significant number of men who undergo pelvic lymph node dissection don’t harbor lymph node invasion by cancer at final diagnosis, the authors explained. Moreover, PLND is associated with complications such as pain, lymphedema, nerve injury, or even blood clots that can cause strokes -- making it important to optimize the indication for PLND, they wrote.
To that end, the researchers investigated whether PSMA-PET scans -- which have a high negative predictive value (NPV) in determining whether cancer has invaded lymph nodes -- can be used to avoid unnecessary procedures in men with intermediate-risk disease.
The group identified 371 patients with available PSMA-PET data for primary staging who underwent radical prostatectomies between 2016 and 2021 at their clinic. The median preoperative prostate-specific antigen level among the group was 7.8 ng/ml. Over a follow-up period of 36 months, the researchers assessed disease-free survival rates among those who underwent pelvic lymph node dissection versus those who did not.
Of the 371, 333 (90%) underwent radical prostatectomy with PLND, while 38 (10%) had no PLND. The median number of lymph nodes removed in patients with PLND was 16 and the NPV of PSMA-PET for detecting lymph node invasion was 90.1%.
According to the analysis, biochemical recurrence-free survival at 36 months was 78.7% for those who underwent pelvic lymph node dissection versus 76.7% (p = 0.8) for those patients who did not have the procedure, the group found.
“In intermediate-risk prostate cancer patients with negative nodal status at PSMA-PET, the performance of PLND does not affect short-term oncologic outcome,” the researchers wrote.
Ultimately, it has been unknown whether patients who are spared PLND based on negative PSMA-PET scans suffer worse oncologic outcomes compared with patients who undergo PLND, the researchers noted. This study addressed this gap in knowledge, they wrote.
“In consequence, the complication-prone procedure of PLND could be spared in selected intermediate-risk patients with a PSMA PET negative for [lymph node invasion],” the group concluded.
The full study is available here.