Making use of imaging features and demographic information, machine-learning algorithms predicted 90-day outcomes in patients with acute ischemic stroke, offering potential as an aid for treatment decisions, according to research published online October 24 in the American Journal of Roentgenology.
A team of researchers led by Yuan Xie of Stanford University developed machine-learning models that could perform reasonably well in predicting patient outcomes based on analysis of stroke biomarkers at admission for acute ischemic stroke. Performance significantly improved, however, with the addition of patient information that's available 24 hours after treatment.
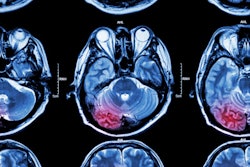
Timely and accurate outcome prediction plays an important role in making decisions on treatment and rehabilitation strategy for patients with acute ischemic stroke. Currently, this decision-making process involves assessment of biomarkers, including imaging features and demographic information, according to the researchers. They sought to use machine-learning methods to integrate these clinical and imaging variables in the acute setting to predict three-month modified Rankin scale (mRS) scores, a measure of disability, in these patients.
The researchers elected to use decision-tree learning, a form of supervised machine learning that is constructed by performing binary tests on a given feature. The initial binary test forks into two new tests, each asking a new question. These questions then form a diverging flowchart, with each end of the branch providing a prediction with a certain confidence level. Ultimately, all of the decisions combine to yield a prediction, according to the researchers.
In a retrospective study, they included 512 patients from a registry of patients with acute ischemic stroke at Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland. Using ground-truth 90-day modified Rankin scale scores in these patients, they trained two types of decision-tree machine-learning models, extreme gradient boosting (XGB) and gradient boosting (GBM), to predict mRS scores using CT angiography and demographic biomarkers available when patients were admitted and 24 hours afterward.
The researchers found that a patient's 90-day mRS score correlated significantly with five biomarkers:
- Scores on the National Institutes of Health Stroke Scale (NIHSS) 24 hours after treatment
- Patient age
- Scores on the Alberta Stroke Program Early CT (ASPECT)
- Presence of hyperdense middle cerebral artery sign (HMCAS) on CT
- The North American Symptomatic Carotid Endarterectomy Trial (NASCET) degree of cervical carotid stenosis
| Area under the receiver operating characteristic curve for predicting 90-day outcomes in acute ischemic stroke patients | ||
| Model | At admission | With selected features & NIHSS score 24 hours after treatment |
| XGB machine-learning model | 0.758 | 0.884 |
| GBM machine-learning model | 0.772 | 0.877 |
In other results, the researchers also found that the models could predict outcomes separately in patients with early recanalization and those with persistent arterial occlusion.
"Prediction of patient recovery based on recanalization status can also help physicians assess the risk and benefits associated with endovascular treatment decisions," the author wrote.
Future work should involve improving multinomial models to specifically predict the modified Rankin scale scores, as well as using image-based predictions to prognosticate recovery outcomes, the researchers noted.
"For larger datasets, other methods, including deep learning, may yield even better results," they wrote.