An ultrasound-based deep learning radiomics nomogram (DLRN) model performed well in a study about predicting tumor status and lymph node metastasis in breast cancer patients post chemotherapy.
The study, published in Academic Radiology on August 24, found that the DLRN model demonstrated high receiving operator curve (ROC) values, as well as moderate consistency in this area, according to researchers led by Sheng-Chun Shu, PhD, from the Second Affiliated Hospital of Guangzhou University of Chinese Medicine in China.
“This fusion model can also predict the prognosis of patients, which could help clinicians make better clinical decisions,” Shu and colleagues wrote.
The ability to predict the effectiveness of neoadjuvant chemotherapy is important for long-term health outcomes in breast cancer patients. Radiology researchers have been studying different methods for better prediction, with AI yielding promise in previous studies.
Shu and co-authors noted that to their knowledge, there has been a lack of data evaluating the combination of deep transfer learning features, radiomic features, and clinical characteristics to evaluate tumor response, as well as axillary lymph node status, to chemotherapy in patients.
They added to the literature, exploring the feasibility of an ultrasound-based fusion model combining the aforementioned features. The team sought to validate the effectiveness of their fusion algorithm and promote clinical use, employing a Cox regression model for survival analysis.
The study included retrospective data collected between 2014 and 2022 from 243 breast cancer patients who underwent chemotherapy. Of the total women, 194 were placed into the training cohort while 43 were placed into the test cohort.
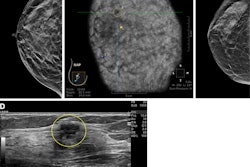
 Feature heat maps based on Grad-CAM. Color-code heat maps overlaid with the corresponding ultrasound images are shown for four patients who were accurately predicted. (a, d) The heat maps highlighted the intratumor region in patients with complete pathologic response or non-lymph node metastasis. (b, c) The heat maps highlighted the peritumor tissue in patients with non-complete response or metastasis. Images are being republished through a Creative Commons license (CC BY-NC-ND 4.0). Image courtesy of Academic Radiology (Elsevier).
Feature heat maps based on Grad-CAM. Color-code heat maps overlaid with the corresponding ultrasound images are shown for four patients who were accurately predicted. (a, d) The heat maps highlighted the intratumor region in patients with complete pathologic response or non-lymph node metastasis. (b, c) The heat maps highlighted the peritumor tissue in patients with non-complete response or metastasis. Images are being republished through a Creative Commons license (CC BY-NC-ND 4.0). Image courtesy of Academic Radiology (Elsevier).
To create the DLRN fusion model, the team used ResNet50, ResNet101, and DenseNet201 models to predict a result and its corresponding probability for each frame for deep learning. For radiomics, the team fused the prediction results of several machine-learning models, including the following: Support Vector Machine, AdaBoost, Multi-Layer Perception, XGBoost, and LightGBM.
The model performed well in both training and test cohorts, including near-perfect ROC curve values in the training cohort.
| DLRN fusion model performance for predicting tumor status and lymph node metastasis, evaluated by ROC (with 1 as reference) | ||
|---|---|---|
| Prediction measure | Training cohort | Test cohort |
| Tumor status | 0.984 | 0.892 |
| Lymph node metastasis | 0.985 | 0.87 |
The nomogram also achieved consistency indices of 0.761 for the training cohort and 0.731 for the test cohort, respectively.
Finally, the Kaplan-Meier survival curves showed that high-risk breast cancer patients had significantly poorer overall survival than women deemed to be low-risk (p < 0.05).
The study authors highlighted that their findings point toward the model being useful for individual prediction in women with breast cancer.
“When clinicians have a more accurate assessment of a patient's survival risk, they are more likely to choose appropriate treatment methods,” they wrote.
The authors added that future research will focus on building larger databases of breast cancer patients, integrating more clinical factors, further improving the predictive model, and conducting multicenter collaborative research.
The full study can be found here.