Supplemental breast ultrasound may have utility in imaging women with dense breasts and high risk of advanced or invasive breast cancer, a study published August 6 in Radiology found.
Researchers led by Brian Sprague, PhD, from the University of Vermont in Burlington found that women at elevated risk of invasive or advanced breast cancer according to established risk prediction models had high supplemental cancer detection rates on ultrasound screening after a negative mammogram, with a moderate positive predictive value of biopsy.
“These findings can help breast imagers estimate the expected outcomes of supplemental ultrasound screening according to a woman’s risk level and assist in determining which women with dense breasts may be good candidates for supplemental ultrasound screening after a negative mammogram,” Sprague told AuntMinnie.com.
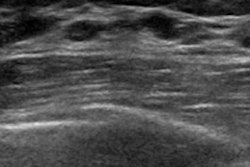
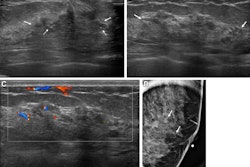
 Sample images show cancer detection at supplemental ultrasound screening after screening mammography with a negative result. (A) Craniocaudal right breast screening mammography shows negative findings in a 54-year-old female patient with extremely dense breast tissue. (B) Coronal view from supplemental screening with automated whole-breast ultrasound image in the same patient four months later shows an irregular hypoechoic mass (dashed yellow circle) in the right breast, diagnosed as invasive ductal carcinoma. (C) Craniocaudal screening right breast mammography shows negative findings in a 74-year-old patient with heterogeneously dense breast tissue. (D) Antiradial gray-scale image in the right breast from supplemental handheld screening ultrasound in the same 74-year-old patient 7 months later demonstrates an irregular hypoechoic mass in the right breast (yellow outline), which yielded a diagnosis of invasive ductal carcinoma. Image courtesy of the RSNA.
Sample images show cancer detection at supplemental ultrasound screening after screening mammography with a negative result. (A) Craniocaudal right breast screening mammography shows negative findings in a 54-year-old female patient with extremely dense breast tissue. (B) Coronal view from supplemental screening with automated whole-breast ultrasound image in the same patient four months later shows an irregular hypoechoic mass (dashed yellow circle) in the right breast, diagnosed as invasive ductal carcinoma. (C) Craniocaudal screening right breast mammography shows negative findings in a 74-year-old patient with heterogeneously dense breast tissue. (D) Antiradial gray-scale image in the right breast from supplemental handheld screening ultrasound in the same 74-year-old patient 7 months later demonstrates an irregular hypoechoic mass in the right breast (yellow outline), which yielded a diagnosis of invasive ductal carcinoma. Image courtesy of the RSNA.
Radiologists are exploring whole-breast ultrasound as a breast cancer screening modality in imaging women with dense breasts. Some prospective trials suggest that ultrasound increases cancer detection rates and reduces interval cancer rates compared with mammography alone.
However, it’s not well known whether supplemental ultrasound screening outcomes in this area vary for women with dense breasts with different levels of breast cancer risk.
Sprague and co-authors sought to add to the literature, evaluating such outcomes for women with dense breasts and different estimated breast cancer risk levels. They included data collected between 2014 and 2020 from 24 radiology facilities within three Breast Cancer Surveillance Consortium (BCSC) registries. This data included ultrasound screening exams from women with heterogeneously or extremely dense breasts.
Final analysis included 34,791 ultrasound screening exams from 26,489 women with an average age of 53.9 years at screening.
The researchers highlighted the following findings:
- The overall cancer detection rate per 1,000 exams was 2.0 and was higher in women with high versus low or average risk of six-year advanced breast cancer (5.5 vs. 1.3, respectively; p = 0.003).
- The overall false-positive biopsy recommendation rate per 1,000 exams was 29.6 and was higher in women with high versus low or average six-year advanced breast cancer risk (37 vs. 28.1, respectively; p = 0.04).
- The overall PPV3 was 6.9% and was higher in women with high versus low or average six-year advanced cancer risk (15% vs. 4.9%; p = 0.01).
The team also observed similar patterns in outcomes by five-year invasive breast cancer risk.
The study authors highlighted that their findings “may provide useful insights to women, clinicians, and policymakers” considering supplemental ultrasound screening strategies in the U.S. This also goes for other countries where national screening programs have implemented ultrasound as a supplement to mammography for women with dense breasts.
“While ultrasound screening does require specific training and expertise, in general, it is a more widely available technology and has higher acceptance among women compared to MRI and other imaging modalities,” Sprague said. “No contrast medium is required.”
Sprague also told AuntMinnie.com that the team is evaluating the potential population-level impact of risk-based supplemental ultrasound screening strategies by using computer simulation models. The models aim to translate these observed short-term screening outcomes into estimates of long-term outcomes, including breast cancer deaths averted and cumulative false-positive exams.
“The results will inform policymakers and healthcare providers as they consider supplemental screening recommendations,” Sprague said.
Risk stratification is important and can improve ultrasound screening outcomes such as those in the study by Sprague et al, according to an accompanying editorial written by Thomas Helbich, MD, and Panagiotis Kapetas, MD, PhD, from the Medical University of Vienna in Austria.
The editorial authors however added that moving from the current age-driven screening approach to a risk-stratified breast cancer screening approach is “not likely to occur at once.” They wrote that it is also important to identify which imaging methods will best serve different patient subgroups.
“Overall, it is a policy of gradualism that will pave the way for supplemental breast screening,” Helbich and Kapetas wrote.
The full study can be found here.