In the annals of American folklore, few stories resonate as deeply as that of John Henry, the “steel-driving man” who challenged a steam-powered hammer to prove human superiority over machines. As the tale goes, Henry won the contest but died with his hammer in his hand, his heart giving out from the superhuman effort. Today’s radiologists face a similarly existential challenge, though its dimensions are not purely mechanical but deeply technological and economic.
 Joshua Ewell, DO.
Joshua Ewell, DO.
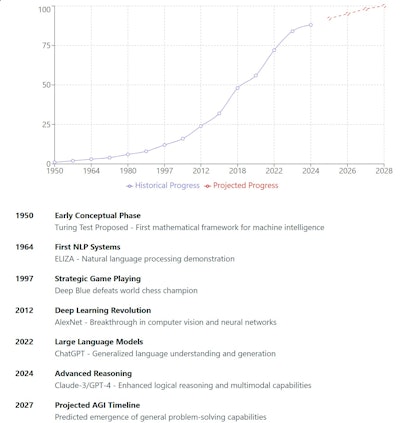
The swift rise of AI and its potential progression into artificial general intelligence (AGI), and even artificial superintelligence (ASI) foreshadow not mere change, but replacement. Unlike the historical clash of steel and muscle, our modern drama unfolds at the intersection of exponential computational power, healthcare economics, and demographic shifts in the radiology workforce.
Some AI pioneers, such as Geoffrey Hinton, have bluntly predicted that radiologists will be among the first to feel the full impact of these developments, suggesting that the field might need to brace for sweeping -- if not outright disruptive -- transformation. To date, radiologists have largely (nervously) laughed off Hinton’s warnings, pointing to the fact that we are still here and working harder than ever -- unconsciously validating his arguments while finding solace in the relief promised by modern AI technology.
A looming crisis
Data from IMV Medical Information Division and the American College of Radiology indicates that, in 2022, about 34,000 (range 30,000 to 37,000) radiologists in the U.S. interpreted around 650 million imaging studies per year. This encompasses 120 million diagnostic X-rays, 91 million CT scans, 42 million MRIs, and 40 million ultrasounds -- numbers that continue to rise at a compound annual growth rate (CAGR) of roughly 4.2% (range 3%-5%, all imaging; 5%-10%, overnight/ER imaging). Projections suggest that by 2030, annual imaging studies could surpass 875 million as a conservative estimate absent significant interventions.
However, which side of this CAGR range will prevail is far from certain. Multiple factors could push growth higher, such as an aging population requiring more imaging paired with heightened fears of malpractice lawsuits in emergency departments. Yet there are also forces that could lower the growth rate: more stringent regulations, insurance constraints, and hospital initiatives aimed at limiting poor resource utilization.
In fact, AI itself may paradoxically work to both expand and contract imaging volumes. While improvements in detection might spur additional screening exams, “smart triage” and protocol optimization software could systematically limit unnecessary scans. Thus, even the trajectory of imaging volumes remains an open question.
Despite ongoing efforts to mitigate ballooning volume, incremental workflow optimizations and telemedicine systems cannot fully reconcile the growing demand with a limited pool of human interpreters. Each modality demands specialized expertise, while hyperefficient scheduling or around-the-clock coverage merely reshuffles the same limited workforce, rather than expanding it.
The demographic cliff
Compounding the volume crisis is a demographic challenge. In 2022, 53% of practicing radiologists were over the age of 55, pointing to a large wave of potential retirements in the next decade. New residency graduates number approximately 1,000 to 1,200 per year, insufficient to offset such attrition. Projections indicate a net workforce decrease of 20%-25% (if not more) by 2030, leaving potentially fewer than 25,000 radiologists to handle an exploding volume of studies.
If we assume that 25,000 radiologists will be responsible for approximately 875 million,000 studies per year, this amounts to an average of 35,000 cases per year, per radiologist; however, the average radiologist currently reads between 16,000 and 20,000 studies per year (80-100 studies/day × 200-250 days/year = 16,000-20,000 studies/year). Assuming an approximate doubling in volume requirements per radiologist within 5 years will place an incredible and predictably unmanageable stress upon an already stressed system.
As competition for radiology talent intensifies, so too does the cost to practices -- yet downward reimbursement pressure undercuts any compensatory rise in salaries. This mismatch signals systemic strain, inviting a solution that some see in AI’s exponential capabilities.
The AI Factor: Narrow AI
Current algorithms cleared by the U.S. Food and Drug Administration (FDA) illustrate the capabilities of “narrow AI,” tools highly effective at well-defined tasks: detecting pulmonary nodules, highlighting skeletal fractures, and identifying and quantifying brain bleeds, for example. These systems augment rather than replace human readers, making it enticing to assume that AI’s functional limitations merely offer a productivity boost through the automation of noninterpretive or low-risk interpretative skill sets. Often, these algorithms achieve accuracy rates that approach but do not surpass those of human radiologists.
Agentic AI as a transitional phase
The next frontier is “agentic AI,” capable of end-to-end interpretation of certain imaging workflows, such as screening mammography or chest x-rays. These systems operate with minimal human oversight once deployed and will begin to see utilization across the workforce in the next one to three years with increasing market purchases. While still domain-specific in many respects, agentic AI should be viewed as a transitional phase between narrowly specialized algorithms and the broader capabilities that future AGI/ASI might bring. In other words, as these agentic systems scale up and incorporate more advanced multimodal understanding, they could evolve -- and eventually converge with (or pave the way for) full AGI or ASI.
Importantly, this progression does not imply that all radiologists will vanish in the immediate future. Rather, we may see a staged move from AI-based “coreading” (serving as a secondary check, especially for high-volume or after-hours work) to more autonomous reading -- starting in settings such as overnight or emergency radiology before expanding into daytime general practice and, eventually, subspecialty domains like complex MRI. The key concern here is the steadily shrinking scope of human-driven interpretation, not its instantaneous extinction.
AGI and ASI: Not just LLMs
The true transformative (and, for many, alarming) possibility lies in the advent of AGI -- AI that matches or exceeds human-level performance across broad tasks. Geoffrey Hinton, a key pioneer in deep learning, famously remarked in 2016 that we should “stop training radiologists” because machine learning might soon outperform them at image interpretation, with a time frame of five to 10 years.12
Recently, in a 2023 “60 Minutes” interview, he clarified that he had been “off by a factor of two,” suggesting that his initial timeline was still too conservative.19 Other prominent thought leaders in this space, such as Sam Altman and Dario Amodei, have predicted AGI might emerge as soon as 2027.
Yet AGI/ASI may not be achieved solely through large language models (LLMs). Some researchers argue that entirely different architectures or paradigms are necessary. For instance, Yann LeCun, Chief AI Scientist at Meta and a pioneer in deep learning, has emphasized that “large language models alone won’t suffice for human-level AI” and has proposed energy-based models as part of a more robust framework for reasoning and planning.17
In an interview, LeCun suggested that while LLMs capture statistical patterns in text, they lack core mechanisms like hierarchical planning, memory, and the ability to learn how the world works through observation and action -- all of which he deems essential for achieving human-like intelligence.17
If, or rather, when AGI arrives, the leap to ASI (artificial superintelligence) could follow rapidly, creating systems more versatile and self-improving than their human counterparts. At this stage, the economic calculus becomes stark: If AGI and/or ASI can reliably perform radiology’s interpretive tasks (and likely more), market forces will exert immense pressure to replace the bulk of human labor in all interpretive domains.
This solution, however, will not come as the result of AI firms’ undue influence over the U.S. medical system but as a welcomed response to the significant pressures applied to the medical system by the complex nature of negative market forces influencing our specialty.
Part 2 of this series will discuss economic pressures, philosophical and spiritual implications, and closing thoughts on the future of AI in radiology.
Joshua Ewell, DO, is the medical director for Synergy Radiology, a teleradiology division of Summit Radiology in Fort Wayne, IN, and Spectrum Radiology in Maine. The opinions expressed in this editorial are his own and do not represent the views of his employer.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.
References
- IMV Medical Information Division. 2023 Imaging Market Outlook Report. Published December 2022.
- Agarwal S, et al. The Radiologist Workforce in 2035: Variation, Disparities, and the Current State of Pipeline. J Am Coll Radiol. 2021;18(4):511-519.
- Kaplan DA. Survey Says: Radiologist Income, Productivity Stabilizes Post-COVID. Diagnostic Imaging. 2023.
- Kulkarni S, et al. Artificial Intelligence in Radiology: The State of the Art and Future Directions. J Am Coll Radiol. 2023;20(1):146-154.
- Medicare Payment Advisory Commission (MedPAC). Report to the Congress: Medicare Payment Policy. Published March 2023.
- Larson DB, et al. Use of an Enterprise Imaging Platform to Assess Radiologist Productivity and Report Turnaround Time. J Digit Imaging. 2022;35(1):188-196.
- American College of Radiology. ACR Commission on Human Resources Workforce Survey. 2022.
- Harvey HB, et al. The Future of Radiology: Artificial Intelligence and Advanced Technologies. RadioGraphics. 2023;43(3):e230017.
- Society of Interventional Radiology. Annual Workforce Survey Report. 2023.
- Bureau of Labor Statistics. Occupational Employment and Wage Statistics: Radiologists. Published May 2023.
- Langlotz CP. Will Artificial Intelligence Replace Radiologists? Radiology: Artificial Intelligence. 2019;1(3):e190058.
- Hinton G. [Interview discussing AI’s impact on radiology at the Royal Bank of Canada (RBC) Conference]. 2016.
- Ng A. “AI Transformation in Healthcare.” Paper presented at: MIT Technology Review EmTech Digital Conference; 2018.
- Topol E. Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. Basic Books; 2019.
- Hassabis D. Keynote lecture. DeepMind Summit; 2021.
- Ridley E. How many studies should a radiologist read per day? AuntMinnie.com. 2018.
- LeCun Y. [Interview discussing energy-based models and limitations of LLMs]. Paraphrased from public statements in various talks and articles; see also: LeCun Y. “Path to Autonomous Machine Intelligence.” Meta AI Blog. 2022.
- Altman S. “I always wanted to write a six-word story. here it is: near the singularity; unclear which side.” [Post on X]. Published January 5, 2025. Accessed January 5, 2025. https://x.com
- Hinton G. The Godfather of AI: Geoffrey Hinton warns of the technology’s dangers. Interview with 60 Minutes. Video posted on YouTube; May 21, 2023. Accessed January 5, 2025. https://youtu.be/qpoRO378qRY?si=-FLWCGesrLBJMnlC



















