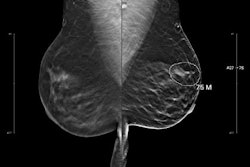
Radiologists must understand how to clearly define the separation of the roles between AI systems and radiologists, suggested an editorial published July 29 in Radiology.
The paper comes as the radiology community faces difficult decisions about how to proceed with integrating AI into workflows, according to Pranav Rajpurkar, PhD, associate professor of biomedical informatics at Harvard Medical School, and Eric Topol, MD, a cardiologist and founder of Scripps Research Translational Institute.
Challenging prevailing views that human radiologists work "with" AI systems, recent evidence demonstrates that integrating assistive AI does not always yield improved diagnostic outcomes, according to Rajpurkar and Topol.
Instead, "role separation leverages the distinct strengths of AI and radiologists by assigning them complementary yet separate responsibilities in the diagnostic workflow," the duo noted. Importantly, they explained that the most pragmatic path forward involves a careful, measured approach to role separation.
Rajpurkar and Topol proposed a framework of three distinct models. They favored the "case allocation model" of triaging cases based on complexity and clarity. In this model, some cases would be managed entirely by AI, others by a radiologist, and the rest managed through a combination.
In the case allocation model, three distinct pathways have emerged, according to the authors:
- AI to rule out normal cases
- Risk-based reader allocation
- Dynamic complexity-based allocation
Another model they referred to as the "doctor-first sequential model." This is where the radiologist initiates the diagnostic process while AI performs complementary tasks such as report generation and follow-up recommendations, the team explained.
"This model acknowledges that certain aspects of radiologic work -- particularly those requiring complex pattern recognition, clinical judgment, and integration of contextual factors -- remain best suited to human expertise," Rajpurkar and Topol wrote.
Promising applications have emerged in the doctor-first sequential model, such as AI systems that synthesize radiologists' detailed findings into concise, structured impressions that include specific diagnoses and management recommendations, they noted.
The third model, an "AI-first sequential model," involves AI processing the initial segment of the workflow (e.g., preparing clinical context from electronic health records). Radiologist interpretation would follow. However, substantial improvements in context management capabilities will be necessary before these systems can be widely deployed in clinical radiology workflows, according to Rajpurkar and Topol.
"Radiologists are stuck in the worst of both worlds -- afraid to trust AI fully, but too reliant to ignore it," Rajpurkar told the RSNA. "Clear role separation breaks this cycle."
"Rather than merging efforts into a single, integrated process -- which can lead to issues like automation neglect and automation bias -- this approach divides the workflow into segments best suited to each party’s unique capabilities," Rajpurkar and Topol explained in their paper.
Ultimately, "current evidence suggests that neither fully integrated assistive approaches nor complete automation represent optimal solutions," they wrote.
"We’re providing a framework, but the real innovation will come from frontline radiologists adapting it to their specific needs," they said. "Institutions will likely discover hybrid approaches we haven’t even imagined yet."
Rajpurkar and Topol also suggested establishing a clinical certification pathway for AI systems.
Read the commentary here.