A new Web-based application takes less than a minute to tell physicians if the transthoracic echocardiography (TTE) test they're pondering is appropriate for the patient. A feasibility study presented at the recent American Society of Echocardiography (ASE) meeting in San Diego showed that it can potentially save doctors and patients a lot of time, money, and heartache.
"There's been a dramatic increase in the number of imaging tests ordered, and costs are rising from both the government and third-party payors' perspective," said R. Parker Ward, MD, in an interview with AuntMinnie.com. "As a result, the government has really been focused on imaging as a priority for reducing costs."
The U.S. Centers for Medicare and Medicaid Services (CMS) recently implemented across-the-board cuts in payments for cardiac imaging services including nuclear stress and echocardiography, said Ward, a cardiologist and associate professor of medicine at the University of Chicago.
The prospective feasibility study was aimed at determining if a Web-based application could sort through the appropriateness criteria quickly and reliably. Ward and his team assessed indications for outpatient TTE studies performed in the university hospital's echocardiography lab using appropriate use criteria for TTE.
The application was developed using the group's own prior published data regarding indication frequency to minimize both the time and the number of screens the staff members would have to work their way through to arrive at a final appropriateness determination for a patient, Ward said.
Even laid out compactly, the written appropriateness criteria exceed 50 pages. That's quite a lot to deal with before an exam, he said.
"If you're busy and ordering a study in your office, you don't have time to flip through page after page of this," Ward said.
On the other hand, the Web tool is designed to enable doctors to get an answer with just a couple of mouse clicks. The researchers recorded the application entry time for 30 of the more than 200 studies they entered.
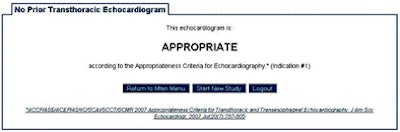
 |
| Screenshot from the APEGS program developed by Ward and colleagues in cooperation with the ASE from the prototype Web-based tool used in the study. Image courtesy of R. Parker Ward © American Society of Echocardiography. |
"A lot of people wrote criteria published in 2006, 2007, and 2008," Ward said. "The question is: Can they be applied to clinical practices in a way that reduces the inappropriate utilization of imaging?"
Indications determined by the prototype Web tool were compared to blinded investigator-determined indications based on review of relevant medical records at the point of care, Ward said. The application asks about indications such as shortness of breath, chest pain, abnormal electrocardiogram tests, for example, and what tests the patient has had in the past.
Repeat tests
The most common inappropriate studies relate to repeat testing, which happens most often when patients undergo an appropriate echo study that is then followed by an inappropriate repeat exam in six months or a year, Ward said.
A lot of inappropriate ordering happens when the first study shows some heart weakness -- for example TTE demonstrates a mildly low ejection fraction -- and a new test is ordered six months later, "even if the patient is fine and there are no new clinical symptoms," Ward said.
Repeat studies can certainly be indicated when the dysfunction is severe, Ward added, but they are often ordered when the abnormality is mild.
The study found that Web-tool-based TTE indications were appropriate (A) in 77% (n = 198) of studies, inappropriate (I) in 9% (n = 23), and not classified (NC) by the area under the curve of TTE in 14% (n = 37), with excellent (94%) agreement between the application-based and investigator-based results.
"The number to focus on is the 9% inappropriate studies," he said. "In general, about 10% of studies are inappropriate," so the application reflects that reality, he said. The reason for the 14% NC rate is that the current appropriateness document "doesn't address all of the indications for echo," he said.
Ward cited at least three reasons driving inappropriate ordering, which include a lack of knowledge of the most recent appropriateness criteria, and the practice of defensive medicine to ward off potential malpractice litigation.
"The third would be incentive-based abuse of ordering -- we'd be naive to think that's not part of it," Ward said.
Appropriateness tools
Well-designed appropriateness tools can help address all three causes of inappropriate ordering, he said. First, they offer a measure of protection to physicians by ensuring that they're treating patients appropriately.
"Frankly they give insurance companies the same protection," he said. "Everyone assumes that insurance companies' goal is to limit testing as much as possible, but if you've got a physician-developed set of criteria that are really about the patient and what is appropriate and what is best care, patients and insurance companies and physicians can all point to that as something to help arbitrate the right time frame."
New appropriate use criteria from the American College of Cardiology Foundation are expected by the end of this year, hopefully in the fall, he said. Meanwhile, the prototype Web tool is being refined as a commercial application known as APEGS.
Using the prototype tool, "we've shown these criteria can be implemented in clinical practice," Ward said.
"It allows an easy, fast, and feasible way to apply appropriate use criteria at our point of service in the echo lab," he said. "It could also be expanded to the point of ordering."
Once APEGS is integrated into facilities' electronic medical record, questions regarding previous studies and other patient-specific information could be populated automatically, further speeding up the process, Ward said.
By Eric Barnes
AuntMinnie.com staff writer
June 21, 2010
Related Reading
Order-entry system reduces inappropriate outpatient exams, June 1, 2010
ACR offers imaging appropriateness app, April 14, 2010
Could decision-support software help radiology fend off RBMs? April 7, 2009
Decision-support software cuts imaging procedure volume, March 24, 2009
CT protocol ordering software increases efficiency, January 29, 2009
Copyright © 2010 AuntMinnie.com


















