CHICAGO - The American College of Radiology's (ACR) Dose Index Registry (DIR) pilot project, launched in May, has already amassed a critical number of studies, while developing ways to keep the data accurate despite wide variations in practice patterns and study nomenclature, according to a Wednesday presentation at the RSNA 2011 informatics sessions.
By accurately tracking medical imaging doses for CT studies, DIR has the ability to establish national benchmarks, enabling individual practices to monitor dose indices and compare practice patterns. Perhaps best of all, it's ready to use now, and any imaging facility can register and help further the ACR's efforts, said Richard Morin, PhD, an ACR fellow from the Mayo Clinic in Jacksonville, FL.
Radiation exposure in the use of medical imaging procedures in the U.S. has been a recent concern of radiologists, medical physicists, healthcare providers, and the public in general, Morin said. Spurred in particular by the publication of the National Council on Radiation Protection and Measurements' (NCRP) Report No. 160 in March 2009, which showed the fast-rising use of medical radiation, the registry represents a major effort to categorize and compare radiation doses across the U.S.
The job is harder than it might seem. Despite significant improvements in CT acquisition and dose reduction technologies, comparing and monitoring doses delivered from CT scans across facilities remains difficult and time-consuming, said Morin. But the registry has already come up with important information that didn't exist before.
"If you asked what is the average radiation dose for a CT administered to the head, as we did several years ago in JACR, the answer would have been 'I don't know,' " Morin said. "We know that it's not 15 Sv, and we know it's not 0.0001 mSv," he said. But what it actually is we don't know. There are surveys that have been done from time to time, but we don't precisely know the number."
Thus was born the effort to register and compare medical radiation doses. "It is a way for facilities to measure their dose index, and compare those dose indices to other areas of the country, other areas of the state, and [other areas of] the world, for that matter," he said. "Now it will be possible for facilities to see where they are, and then make decisions about whether to change their CT techniques to reduce the dose and still have high image quality."
The National Quality Forum has approved the registry for meaningful use applications, and it is expected to be adopted soon for maintenance and certification, he said.
"Registries are very good ... in terms of being able to gather data, look at national benchmarks, analyze your results, and develop a plan for how to change them in the future," he said.
The DIR is a component of the National Radiology Data Registry, Morin said. It collects and compares dose information across facilities using standard methods of data collection, such as DICOM Structured Reporting and Integrating the Healthcare Enterprise (IHE) Radiation Exposure Monitoring (REM) profiles, and establishes national benchmarks and practice patterns in dose indices.
"Most importantly, there's no human intervention," as the data are transmitted automatically once the software is installed, Morin said. The data are sent to a computer that is equipped with an ACR software application that anonymizes the information, extracts what is necessary (primarily CT dose index volume [CTDIvol] and dose-length product [DLP]), and uploads it to a database, he explained. Reports are then generated, and the facility can compare their results.
To participate, a facility can sign up via a link at the ACR's website, sign a participation agreement, pay a fee, and then have its CT scanners configured to send data to the program, Morin said.
By mid-June 2011, a total of 1,944 exams had been mapped to one of five exam types: head CT with contrast, head CT without contrast, chest with contrast, chest without contrast, and head CT perfusion. Significant differences (p < 0.05) in CTDIvol by facility were found for all exam types except head CT perfusion, which had only 20 exams to compare at the time. The range of dose indices varied from a factor of six to a factor of 368.
All told, about 300 institutions have registered since May, and approximately 125 are active, Morin said. Foreign participation from Brazil, Canada, Spain, Ireland, Argentina, Switzerland, and New Zealand is helping to internationalize the project, and there has been a lot of interest during the RSNA meeting as well, according to Morin. More than 500,000 individual scans have been transmitted to date.
A head CT by any other name
During the pilot study, it became clear that people don't call the same exam by the same name. "In fact, what you think would be pretty straightforward -- a head scan or a brain scan -- actually in the registry right now has 1,400 different names for what we think are head scans," Morin said.
CT head without contrast alone generates 224 different names from 60 facilities representing 20,677 exams, "so the nomenclature is extremely important," he said. Participating facilities are adopting the RadLex playlist nomenclature for their CT exams via software on the website.
The other important variable is body habitus, and efforts are under way to get size-specific dose estimates by the first quarter of 2012.
CT head scans, dose results for first 6 months of DIR
|
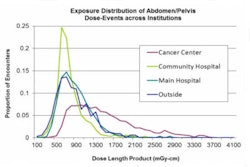
Facilities can download the dose information via Microsoft Excel spreadsheets by scan or by exam. The facility gets the mean and median of their individual data, and they can then compare that in other ways -- by location, by type of practice, by geographical region of the country, or by the entire dose index registry, Morin said.
A facility's outlier exams can be identified using the registry's dose distribution charts. There may be good reasons why the dose increased, but it offers facilities a chance to look at the dose outliers, figure out how it happened, and make a plan to change things, Morin said.
"We are getting new facilities every week, exam standardization is going on, reference levels are coming, and we expect to have the patient size in place at the beginning of next year," he said.