VIENNA - "The OR (operating room) of the new millennium is likely to be a hybrid OR; that means something in between a radiological suite and a conventional surgical room," remarked Prof. Andrea Pietrabissa, director of general surgery, Policlinico San Matteo at the University of Pavia, Italy. "That shift has already occurred with vascular surgery, where endovascular techniques are quickly changing surgical practice."
Today, intraoperative imaging is mostly limited to C-arm x-ray and ultrasound; use of intraoperative CT and MRI is restricted due to environmental constraints and incompatibility with the use of metal-based surgical instruments. However, more integration between preoperative studies and intraoperative images and views is already possible, and technical fusion of these should be considered when designing new operative rooms.
"These steps represent the bricks upon which intraoperative navigation can be built," stated Pietrabissa. "We should also consider robotic surgery as the main IT revolution that has already occurred in general surgery ORs. This technology incorporates several new features, including the possibility to fuse images, and that of remote tutoring and counseling."
 |
| Coming to an operating room near you? Consoles like these look set to become more commonplace in the future. (Provided by Prof. Andrea Pietrabissa) |
Integrating the OR with IT systems can have a positive impact on many aspects of surgery, including its safety. Efficient handling of the flow of data about the individual patient by OR personnel is crucial in avoiding human error and limiting damage when errors do occur. Risk managers know that a digital OR is a much safer place than a paper-based OR, he commented.
Image-fusion technology looks set to continue to play a significant role in the years to come; this fusion is likely to occur inside the 3D display of new robotic systems and will incorporate new dyes and new camera detectors that are today appearing as early prototypes, Pietrabissa predicted. An example is the capability to visualize the biliary tree with intraoperative injection of indocyanine green and the simultaneous use of a robotic infrared camera, coupled with the conventional 3D robotic camera.
 Risk managers know that a digital operating room is a much safer place than a paper-based OR, according to Prof. Andrea Pietrabissa.
Risk managers know that a digital operating room is a much safer place than a paper-based OR, according to Prof. Andrea Pietrabissa.
"This new technology is able to provide a realistic 3D vision of the biliary anatomy during the procedure, and is potentially capable of limiting surgical injuries to the biliary system. It is expected that intraoperative guidance with similar markers will soon be available also for the most important area of cancer detection and lymphatic sampling for staging purposes," he said.
Intraoperative imaging has become steadily more popular since the early 1980s. For instance, intraoperative ultrasound of the liver is now routinely used to identify the limits of liver tumors, and to detect the main intrahepatic vessels. Laparoscopic ultrasound is also widely used to stage gastrointestinal cancer and to detect occult pancreatic and liver tumors.
"Both diagnosis and treatment are today image-based and driven," explained Pietrabissa. "Most of our patients undergo ultrasound, CT, MRI, or a combination of these exams before their surgery, not only to diagnose the underlying disease, but also for the purpose of accurately planning the procedure."
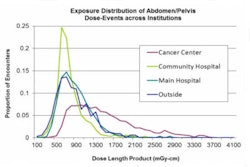
In addition to providing practical information about intraoperative imaging, this morning's refresher course will demonstrate how the adoption of digital image management by disciplines and departments outside of radiology for their own clinical purposes is gathering momentum. Large-scale, multidisciplinary image sharing across and beyond campuses puts novel requirements on PACS solutions, and it also raises the key question of how images should be managed effectively. The course aims to summarize the current controversy, present various approaches to PACS design and architecture, and help build an understanding for advanced data management, as well as concrete technical, legal, and workflow aspects.
 Robotics is having an increasing impact on healthcare delivery, particularly surgery. (Provided by Prof. Andrea Pietrabissa)
Robotics is having an increasing impact on healthcare delivery, particularly surgery. (Provided by Prof. Andrea Pietrabissa)
In many healthcare systems, PACS solutions have widely replaced conventional film-based technology and workflow in radiology departments and imaging centers. Image acquisition and reading have gone digital during the past few years. The trend toward image sharing with other colleagues is a logical extension of this process.
Interventional suites provide a perfect example of the crucial role image-based diagnostic and therapeutic workflows have started to play. Image management can significantly support positive outcomes; on the other hand, it is a highly cost-intensive component in clinical settings. In order to ensure that investments will meet growing demands, and implementations will indeed help optimize workflows, decision-makers in care provider organizations need an understanding of workflows and information and communication technologies for image management.
Communication, simulation, visualization, and navigation of images are becoming essential features in the planning and implementation of complex PACS infrastructures in support of diagnostic and interventional procedures. "While the full potentialities of multidisciplinary image sharing within healthcare settings are being further explored, it is now increasingly common to see intense cooperation between radiologists and other clinicians for planning and guiding interventions," noted Prof. Dr.-Ing. Heinz U. Lemke, who will be chairing the course. He is a research professor of radiology, University of Southern California, Los Angeles, and professor of computer-assisted surgery at the University of Leipzig in Germany and director of the International Foundation for CARS (Computer-Assisted Radiology and Surgery).
During the course, "New PACS architectures: decoupling image management from image navigation," the lecturers will give insights into image sharing, from hospital-based PACS applications to remote consultation, with specific reference to the support of surgeons regarding training and intraoperative guidance.
Originally published in ECR Today March 5, 2012.
Copyright © 2012 European Society of Radiology