
In those years, nothing suspicious had been detected in the shadowy presentation of her unusually dense breasts, and, again, nothing appeared on mammography images acquired in the Mayo Clinic trial. But when she was examined with molecular breast imaging, an intensely bright focus, indicative of a large lobular cancer, appeared on the images.
MBI uncovered five other cancers that escaped detection with mammography in the trial, but the memory of this patient persisted for Carrie Hruska, PhD, an associate consultant in medical physics at the Mayo Clinic in Rochester, MN, as she presented preliminary results from the trial at the American Society of Breast Disease (ASBD) meeting in New York City in April 2010.
"I can safely say that we saved her life by screening with MBI," Hruska said.
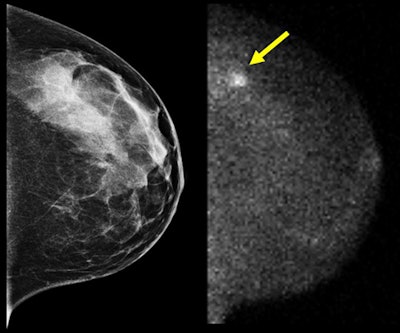
A 45-year-old woman with elevated risk for breast cancer due to breast density underwent digital screening mammogram (left)
and screening MBI (right) as part of a clinical trial.
A biopsy from the area of suspicious technetium-99m (Tc-99m) sestamibi uptake (arrow) indicated the presence of a large lobular
carcinoma. All images courtesy of Carrie Hruska, PhD.
A new arrival
MBI is the latest arrival in a new generation of functional breast imaging technology designed to overcome the limitations of anatomic breast imaging.
Though mortality rates have declined, breast cancer remains a nefarious disease. In the U.S. alone, it killed more than four women every hour of every day in 2006, the last year for which complete data are available.
It is no secret that cases escape notice through holes in the current diagnostic armamentarium of screening x-ray mammography, diagnostic mammography and ultrasound, and breast MRI. Practitioners and patient advocates complain that too many interval cancers are missed and too many benign or non-life-threatening masses are biopsied and treated.
MBI may help fill the breach. Early work took place at Mayo, which has licensed its technology to Gamma Medica (GMI) of Northridge, CA, for commercialization. Multimodality vendor GE Healthcare of Chalfont St. Giles, U.K., announced in June that it, too, is investigating MBI.
MBI shares family ties with other functional approaches to breast imaging, including breast-specific gamma imaging (BSGI) and positron emission mammography (PEM). All three capitalize on diagnostic nuclear imaging methods.
MBI and BSGI employ gamma cameras specifically designed for breast examination using technetium-99m (Tc-99m) sestamibi, the preferred radiopharmaceutical probe for tumor localization and imaging. Tc-99m is the workhorse radioisotope for such single-photon imaging. Sestamibi concentrates in cells with increased mitochondrial density, a common condition for metastatic breast disease.
PEM is a breast-specific version of a PET camera. Procedures are performed with fluorine-18 FDG, a sugar analog that is avidly metabolized as an energy source for cancer cells.
MBI, BSGI, and PEM are all designed as more diagnostically specific and less expensive alternatives to breast MRI, the current gold standard for diagnosing and evaluating difficult breast cases, especially women who have highly dense breasts or carry BRCA1/BRCA2 mutations that make them genetically susceptible to early-onset breast and cervical cancer.
The American Cancer Society (ACS) recommends MRI and mammography screenings annually for women at high risk of breast cancer, classified as greater than a 20% lifetime risk. It advises women at moderately increased risk (15% to 20% lifetime risk) to discuss the potential value of MR screening with their doctors.
Though no definitive clinical trial has been published for any of the functional technologies, preliminary studies suggest they perform well for claustrophobic women who don't tolerate MRI, and for women who harbor metallic implants that are contraindicated for MRI.
MBI proponents believe that it could first have a role in breast cancer screening for at-risk populations, and possibly later aid older women in the general population. The realization of that vision could lead MBI into the mainstream of breast imaging, a goal that neither BSGI nor PEM have yet realized. But MBI developers acknowledge they will have to reduce the radiation dose from MBI before it will be acceptable for screening use.
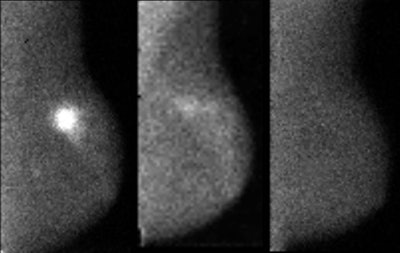
A 51-year-old patient diagnosed with triple-negative, stage II invasive ductal carcinoma measuring 3.5 cm at greatest extent. The image at left is MBI performed prior to beginning neoadjuvant chemotherapy. The middle MBI image was taken three weeks after initiation of chemotherapy (Taxol and carboplatin) and shows near-complete interval resolution of tracer uptake within the tumors, indicating good imaging response to chemotherapy. The MBI image at right was acquired after four months of chemotherapy and is negative, indicating complete response. At surgery, no residual disease was found.
A clinical evolution
Molecular breast imaging represents an evolution of work done on scintimammography starting in the 1990s, when investigators began performing Tc-99m sestamibi scans on general-purpose gamma cameras. But scintimammography never caught on with breast imaging practitioners, according to Michael O'Connor, PhD, a medical physicist at Mayo who has conducted early work on MBI.
The highest resolution possible during functional imaging occurs within a few millimeters of the scanner's collimator and detector, according to O'Connor. Optimizing resolution on a conventional gamma camera during scintimammography proved impossible because the patient had to be imaged in a prone position. The ability to detect small tumors was limited because the breasts were about 15 cm from the collimators and up to 25 cm from the region of interest.
The breasts could also only be visualized from the lateral side and anterior/posterior views. Side-by-side correlations with the craniocaudal and mediolateral oblique views acquired from mammography were difficult.
The new functional breast imaging scanners overcome these problems by reducing the size of the detector and integrating it into the breast compression device. The breast presses against the collimator/detector face while the patient is imaged in a seated position.
The use of matched, solid-state cadmium zinc telluride (CZT) detectors in a dual-head configuration helped O'Connor and colleagues at the Mayo Clinic to optimize detector geometry for their MBI system laterally through the breast, and it improved the typical 3- to 4-mm resolution expected from such a camera to 1.6 mm. Each square hole in the tungsten collimator is matched with a pixel in the detector and optimized for imaging objects within 3 cm of the collimator surface. Each CZT detector is positioned with an individual pixel element, O'Connor said.
MBI can detect lesions as small as 3 mm in diameter, according to O'Connor. Its sensitivity to tissue abnormalities with diameters of 5 mm to 20 mm is 90%.
"A key component in our design was optimizing our ability to detect tumors 5 mm to 10 mm because of the importance of lesions in that range of sizes for the patient's prognosis," he said.
The capabilities have been integrated into the LumaGem scanners commercialized by Gamma Medica. The firm secured U.S. Food and Drug Administration (FDA) 510(k) clearance to market the MBI configuration in December 2009, and commercial shipments began this summer.

The LumaGem molecular breast imaging (MBI) camera is a dedicated breast imaging system with cadmium zinc telluride (CZT) digital detectors.
In contrast, another functional breast imaging technology, the Dilon 6800 BSGI scanner from Dilon Diagnostics, uses a single detector head with pixelated sodium iodide scintillator technology, according to Doug Kieper, vice president of science and technology at the Newport News, VA, firm. An array of position-sensitive photomultiplier tubes (PMTs) gives the system the ability to localize an event within a single PMT to within 0.1 mm. Each PMT has the ability to identify the location of scintillation events without needing Anger logic, the localization method used in conventional gamma cameras.
San Diego-based Naviscan, the leading commercial developer of positron emission mammography, has incorporated many of the patient positioning and resolution features found on MBI and BSGI into its PEM scanner. Promoted as an alternative to breast MRI, PEM detects breast tumors as small as 2 mm in diameter.
Clinical experience
BSGI is typically used for recently diagnosed cases in the same way MRI is used: to look for multifocal and multicentric disease after diagnostic mammography and ultrasound, but before biopsy, according to Lillian Stern, MD, an assistant professor of radiology at Thomas Jefferson University and director of the Women's Health Center at Methodist Hospital in Philadelphia.
A small role has been carved out for BSGI since its installation at the breast imaging center four years ago. About five BSGI procedures are performed there every week to look for disease after diagnostic mammography and ultrasound when MRI can't be used. During long-term follow-up, it is performed to differentiate between malignant recurrence and scarring from previous surgery, she said.
BSGI also substitutes for MRI for monitoring the response to adjuvant chemotherapy before surgery. After a baseline scan, it is performed immediately after a three- and six-month regime of chemotherapy depending on the case and the preferences of the oncologist, she said. The lack of sestamibi uptake correlates with a positive response before mastectomy. High uptake correlates with progressive disease or a partial response. In those instances, the findings suggest that the oncologist should shift to a different chemotherapy after surgery, Stern said.
SNM of Reston, VA, announced in June guidelines covering seven diagnostic indications for BSGI. They include initial breast cancer staging; investigating suspected recurrence; indeterminate abnormalities, such as nipple discharges; imaging of dense or augmented breasts; and cases involving MRI contraindications.
The Mayo group is also gaining experience with MBI for monitoring treatment. Several trials are under way, including a pilot project examining the value of MBI performed before and after neoadjuvant chemotherapy administered before mastectomy.
"Results were encouraging," Hruska said. "We showed, especially among dense-breasted women, that we could accurately predict response to therapy compared to mammography for the same role."
PEM plays many of the same roles where it has been applied, said Wendie Berg, MD, PhD, a breast imaging radiologist in Lutherville, MD.
Cohort studies examining women with known or suspected breast cancer suggest that PEM's performance is similar to MRI. Studies have shown that its specificity is slightly better than MRI, she said in an interview.
A 2006 trial by Berg, for example, established sensitivity and specificity rates for PEM at 90% and 86%, respectively. She was encouraged by the 88% positive predictive value for determining noninvasively whether a suspicious lesion was cancer.
MBI and cancer screening

While MBI aims to develop into a substitute for breast MRI for evaluating known cancers, the Mayo group is looking to expand the technology's role to breast cancer screening for high-risk women, as witnessed by the research Hruska presented earlier this year in New York City.
The study, conducted by lead author Deborah Rhodes, MD, of the Mayo Clinic, involved 936 at-risk women and MBI performed with blinded interpretations. In preliminary results reported last year, Rhodes indicated that the sensitivity of mammography alone for these difficult-to-image patients was 27%, while the sensitivity of combined mammography and MBI was 91%.
Eleven participants were diagnosed with breast cancer. One cancer was only seen on mammography, and seven were detected only with MBI. Two appeared with both modalities. One was missed by both, to be detected a year later. A paper on the research has been accepted by Radiology, and Rhodes will also present the paper at the upcoming RSNA meeting in Chicago.
"The results suggest that MBI can detect more cancers than mammography in dense breasts," Hruska said.
Questions on radiation exposure
But before MBI or any other functional breast imaging modality can be used in a screening role, issues regarding radiation dose will have to be addressed.
In a study released on August 24 ahead of print for the October 2010 edition of Radiology, R. Edward Hendrick, PhD, a clinical professor of radiology at the University of Colorado-Denver in Aurora, concluded that a single BSGI or PEM exam carries a lifetime risk of inducing fatal cancer that is greater than the risk from a lifetime of annual screening mammography starting at age 40.
Hendrick, a medical physicist who advised the FDA on safety standards for the agency's mammography accreditation program, identified a huge difference in the effective radiation dose from mammography, which involves a dose of no more than 0.56 mSv, and the two functional breast imaging techniques. The BSGI and PEM procedures involve effective doses of 6.2 mSv and 9.4 mSv, respectively, he wrote. The average annual dose from natural background radiation is 3 mSv.
MBI was not included in his study, but Mayo's screening trial involved procedures that exposed subjects to 20 mCi of radioisotope, a quantity that O'Connor said translates into an effective dose of 6.5 mSv.
Andrew Karellas, PhD, a professor of radiology at the University of Massachusetts Medical School in Worcester, recognizes the potential value of MBI for screening high-risk women, but he believes that dealing with MBI's relatively high radiation dose compared to screening mammography will be challenging. To be workable, the administered dose of Tc-99m will have to be less than one-tenth of the activity reported in Mayo's studies, he noted in written comments to AuntMinnie.com.
"Maintaining an adequate signal-to-noise ratio with this lower administered dose will require careful reassessment of the hardware, particularly the design of the collimator and the acquisition time for attaining adequate photon statistics," he wrote.

O'Connor agrees that the radiation exposure from MBI must be reduced, but he argues that such reductions can be achieved without sacrificing imaging accuracy. In anticipation of the safety requirement for screening, his group has been working on radiation reduction schemes for two years.
At the time of the Rhodes screening study, Mayo was performing MBI with a unit featuring CZT detectors fitted with standard collimators; therefore, researchers had to use a 20-mCi dose of sestamibi to get adequate count rates and image quality, Hruska said. This is simply too high a dose to administer year after year on a screening basis, she acknowledged.
Since then, with the realization of MBI's higher sensitivity in dense breasts compared to mammography, Mayo researchers have redesigned the collimator and made other improvements to support a 4-mCi study, "which would give an effective dose at a comparable level to digital screening mammography," Hruska said.
"Our goal is a 2-mCi study, which would give a radiation dose about the same as tomosynthesis," according to O'Connor.
The Mayo Clinic has started a second screening study to compare the new low-dose MBI protocol to screening digital mammography. Thanks to the new design, researchers are getting better image quality at 4-mCi doses compared to the original 20-mCi dose, Hruska said.
Dilon Diagnostics is also developing radiation reduction strategies for its BSGI system. For PEM, screening applications are not under consideration, according to Berg. She believes its exposure levels are acceptable for diagnostic applications because few patients will rarely receive more than a few procedures.
At Mayo, Hruska stresses that more clinical testing is also necessary to validate the positive scientific findings and satisfy anecdotal experiences that exemplify MBI's early use for breast cancer screening.
"There were seven cases in our screening trial where we picked up a cancer with MBI that was not seen on mammography," she noted. "I would say that was a benefit for those women."
By James Brice
AuntMinnie.com contributing writer
September 14, 2010
Copyright © 2010 AuntMinnie.com



















