Bernstein & Associates, Architects
As the U.S. healthcare system struggles to adapt to new government regulations and shifting financial realities (including changing reimbursement rates), one sector that offers a potential helping hand is architecture. Knowledgeable architectural firms offer a useful blend of strategic thinking, practicality, and creativity. For healthcare entities looking to cut costs, maximize staff efficiency, and increase patient satisfaction, our firm created the following 10 points that can be used as a framework for forward-looking healthcare design and construction.
1. Greening the healthcare environment
An important development that has swept across all architectural project types -- and is particularly relevant to healthcare and laboratories -- is the "green design" movement. Simply put, this movement advocates environmentally friendly design on several levels:
- On a macro level, buildings are designed to use fewer natural resources in their daily operations (less electricity, less fuel, less gas).
- Also on a macro level, design specifications avoid depletion of scarce natural materials from endangered environments.
- On a micro level, buildings are designed to be toxin-free to their inhabitants (examples of impacted areas include fresh air requirements and specification of materials that do not emit volatile organic compounds).
To socially conscious hospitals, and particularly as a foundation for a healing environment, the appeal of green design is enormous.
2. Planning for the future
It’s easy to plan for the present. We know what current needs are, what current patient volumes are, and so on. Less easy to project are requirements three or five or 10 years down the road. Yet the best strategy for the initial planning process is to base size and quantities on expected requirements five years beyond the expected project completion date.
Let’s say that a current program dictates a requirement for 100,000 gross square feet (sq. ft.), but that requirements projected for seven years down the road (two years for project completion plus five years past that) are for 135,000 square feet. Then the options are:
- To build 135,000 square feet to begin with.
- To build 100,000 square feet initially, with an understanding of how (and where) 35,000 square feet will be added in the future.
- In this way, the impact on the site, as well as on the mechanical/electrical systems of the combined 135,000 square feet, is predetermined, as is the programmatic and planning relationship between the initial 100,000 square feet and the secondary 35,000 square feet.
3. Extending the useful life of your built environment
Part of extending the useful life of your facility was discussed above; however, another part of this goal is accomplished by decisions made in the selection of architectural and engineering materials and systems. Building materials specified by the architect should be extremely durable, maintainable, and come with a minimum 10-year warranty provided by a company that has been around for at least a decade and is likely to be around for another 10 years.
Similarly, from an architectural detailing perspective, the terminations of materials and the transitions between materials must be handled in a way that maximizes the useful life of those materials. Similar care should be taken in the specifications, detailing, and location of all mechanical and electrical components of the building.
4. Creating an appropriate and appealing environment
A healthcare environment has to serve some important constituencies: patients, families and friends of patients, and staff. In addition, the cultural and demographic range of these constituencies -- depending on the size and location of the facility -- can range from large to enormous. Thus, the demands on the look and feel of the healthcare environment are challenging. So what’s appropriate?
Although some would argue that aesthetics are a personal matter, the argument does not hold true with such a large constituency. Based on our years of experience, we believe there is a correct aesthetic for a healthcare environment. A healthcare environment should not be jarring, or unsettling, or exceptionally dull. The goal of the healthcare environment is neither to provoke nor to dramatically understimulate patients, patients’ families, or staff.
On the contrary, the goal of the healthcare environment must be to comfort, befriend, and charm its visitors and staff. The classic elements of architecture -- form, proportion, texture, and color, all bathed in an appropriate mixture of natural and artificial light -- must be used to create a colorful and appealing environment, which facilitates and augments the healing process.
5. Systems integration
The good architect is a systems integrator. Successfully planned and executed, the final built product in a healthcare setting is a symphony of individual systems wedded together into one super-functional whole. The primary architectural/engineering (A/E) systems are:
- Architectural (exterior "skin" and interior build-out).
- Mechanical/electrical engineering systems.
- Structural systems.
The secondary systems are furniture and equipment.
Some obstacles to this integration are: splitting the A/E design into separate contracts not coordinated by the architect; equipment specifications either not being available during the design phase, or specs that change after the design process is complete; and furniture plans and specifications that are not coordinated by the architect.
6. Proper design methodology
Sometime a client’s schedule does not allow for a proper design methodology, but the correct methodology starts with a program, which is a list of required spaces compiled by the architect, along with required net and gross square footages. With a program approved by the client, the architect compares the program square footage to the available square footage, and if there is a discrepancy, either the program or available space must be adjusted.
With a fit between program and available space, and following the completion of a code study, the architect provides schematic design options, one of which is signed off by the client. The approved schematic is "costed" (i.e., a construction cost estimate is provided) and the construction cost estimate is compared to the client-provided budget -- if there is a discrepancy, either the project scope or the budget is adjusted, prior to commencement of construction documents. Adherence to the above steps helps to assure synchronization between the program, budget, design, and the final built project.
7. Patient dignity, privacy, and comfort
In many ways, these patient-centered goals are the primary goals of any healthcare design. Important factors to patients in their initial choice of a hospital or in making return visits -- beyond the quality of the healthcare and convenience -- are certain universal, if sometimes unstated, patient aspirations.
Try to imagine the entire entry process/exit sequence from the point of view of the patient. An environment that supports patient dignity utilizes signage, proportion, and patient flow in a patient-centered, patient-sensitive manner. Patient privacy is a particularly hot button in healthcare design, and is accomplished by making sure that patient registration areas, treatment areas, and patient record storage are handled in a way that maximizes privacy.
Finally, patient comfort is achieved through an emphasis on ergonomic design, comfortable furnishings, and appropriate lighting with some measure of room-by-room control, as well as properly designed heating, ventilation, and air conditioning (HVAC) systems.
8. Doing more with less
Good architecture helps clients achieve critical goals, and a critical goal of healthcare facilities today is to do more with less. There are three areas that we look to in this regard: reduction of facility capital costs; reduction of facility operating costs; and reduction in staffing costs. In terms of capital costs, it is important to:
- Plan projects in an efficient manner.
- Specify efficient and cost-effective systems (structural, mechanical).
- Specify cost-effective materials (exterior and interior).
A recent value-engineering study we did for a large facility in New York City offered cost-saving suggestions totaling millions of dollars. Decreased facility operating costs are achieved through the design of energy-efficient mechanical/electrical systems and architectural and mechanical systems that can be maintained by a smaller maintenance staff. In addition, staffing costs can be decreased if the facility is designed in a manner that reduces staff travel time, staff procedural time, and staff administrative time.
9. New technologies
New technologies that impact healthcare design fall into two main categories that sometimes overlap. These are new medical technologies and new electronic and communication technologies. Being aware of new medical technologies is important for the architect, as upcoming technologies may have spatial or architectural/engineering system implications for current projects.
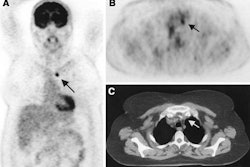
As an example, we are designing all 1.5-tesla MRI suite projects with the capability of being converted to 3-tesla facilities by the client in the future with minimum facility changes. New electronic and communication technologies, of course, are having the same revolutionary impact on healthcare as they are having on other industries (albeit at a sometimes slower acceptance rate in the healthcare industry).
Examples of the impact of these technologies on healthcare include established systems such as PACS and various hospital information systems, as well as upcoming technologies such as wireless communications, bedside registration, and the "digital dashboard" concept for the ER. There is enormous potential for these and other technologies to make the healthcare industry and environment more efficient, more cost-effective, and more patient-friendly.
10. New reality
In the wake of September 11, the new reality is the potential for further terrorist attacks. There is now a need for healthcare institutions to be better prepared for potential attacks directly on their facilities, as well as biological, chemical, or radiation attacks on the general population.
In terms of both protecting hospital buildings and being better prepared to handle a mass casualty event, there are long lists of options and strategies for interested hospitals. Many hospitals, as well as hospital systems, are awaiting government funding, which has been extremely slow in coming. A smaller number of hospitals have engaged architectural firms such as ours to plan and implement preparedness systems, which address these issues.
By William N. Bernstein
AuntMinnie.com contributing writer
February 10, 2003
William N. Bernstein is principal of two architecture and interior design firms in New York City: Bernstein & Associates, Architects (www.bernarch.com) specializing in healthcare, laboratories, and office space; and Architecture for Radiology, LLP (www.arch4rad.com) specializing exclusively in radiology facilities. He is a Yale University-trained architect with more than 20 years experience in the design and construction of specialized, technically demanding facilities in the U.S. and Canada. Bernstein is a member of the American College of Healthcare Architects and the American Institute of Architects, and can be contacted at 212-463-8200 or at [email protected].
Related Reading
Go with the flow: Is your facility designed for maximum utilization?, November 18, 2002
Facility-planning implications of the new MRI safety guidelines, September 9, 2002
MRI design resonates with functional, aesthetic qualities, July 22, 2002
Finding the right space for a new imaging center, July 15, 2002
Copyright © 2003 William N. Bernstein, ACHA, AIA