Two recent radiation therapy studies with different aims have related findings regarding the management of patients that require radiation therapy for cancer. One shows that using whole-body FDG-PET scanning can help stage and manage patients with various types of malignant tumors. The other finds that estimating the number of prostate cancer cases for whom radiation therapy is indicated will help treatment centers gauge the appropriate radiation therapy rate, and plan more effectively for treatment.
Altering treatment goals
In a study published in the Journal of Nuclear Medicine, lead author Dr. Elena Dizendorf and colleagues at University Hospital in Zurich sought to determine the effect of whole-body FDG-PET scanning on the staging and management of cancer patients. They cited PET’s diagnostic accuracy and the established importance of tumor staging.
The investigators reviewed the treatment records of 202 consecutive patients who had different types of malignant lesions. All patients had undergone whole-body PET, and radiation therapy was planned for all of them.
The patients consisted of 98 men and 104 women with an average age of 56.9 years and an age range from eight to 91 years. The investigators found that, for 27% of the patients, the PET results changed the patient management strategy regarding the dose, volume, or intent of radiotherapy.
These results were particularly striking in the head and neck cases, in which therapy changes occurred in 33% of cases. In gynecologic cases, treatment changes occurred in 32%. In breast cancer cases, the treatment protocol was altered in 25% of the cases because of FDG-PET results; in lung cancer cases, there was a change in 31% of the cases.
 |
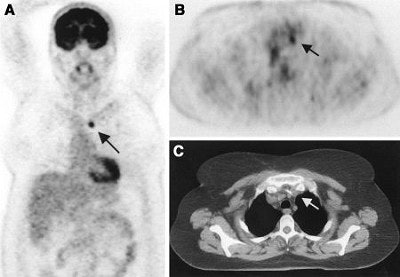
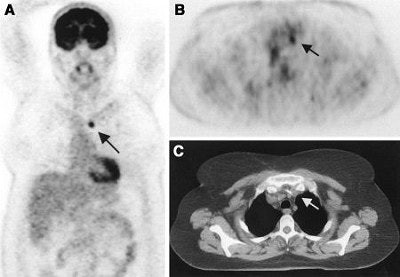
| A 75-year-old woman after resection of rectal carcinoma. Before FDG-PET imaging, curative radiotherapy was planned. Coronal (A) and transverse (B) scans show previously unknown iliac internal lymph node metastasis (arrow). Correlating CT scan (C) does not show any metastases. Treatment was changed from curative to palliative treatment (chemotherapy). Image and caption courtesy of Dr. Elena Dizendorf and the Journal of Nuclear of Medicine. |
"The initial intention of the radiation therapy before PET was defined as curative for 179 patients and as palliative treatment for 23 patients," Dizendorf and colleagues reported. Physicians changed the treatment strategy because of the PET results for 48 (27%) of the 179 patients planned for curative therapy and for seven (30%) of the 23 patients designated to receive palliative treatment (JNM, January 2003, Vol. 44:1, pp. 24-29).
In 18 (9%) of patients, the PET results caused physicians to decide not to perform radiotherapy. Eight had distant metastases, nine had additional lymph node metastases, and active disease was excluded in two patients. In six patients, radiotherapy was cancelled for multiple reasons.
 |
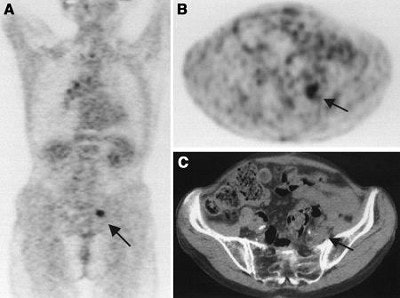
| A 50-year-old woman with lung cancer of right lower lobe. Before FDG-PET, primary curative radiotherapy was planned. Coronal (A) and transverse (B) scans show previously unknown contralateral mediastinal lymph node metastasis (arrow). Lymph node metastasis is not seen primarily on CT scan (C). Radiotherapy volume was increased. Image and caption courtesy of Dr. Elena Dizendorf and the Journal of Nuclear of Medicine. |
In 21 cases (10%), the treatment goal, either curative or palliative, was changed. Clinicians changed the radiation dose in 25 cases (12%). They changed the radiation volume in 12 patients (6%).
The authors stated that because more clinical data need to be accumulated, they are involved in an ongoing study in which they are evaluating the impact of integrated PET-CT on radiation treatment decisions, analyzing their data by tumor type.
Estimating radiotherapy utilization
In a study published in the most recent issue of International Journal of Radiation Oncology, Biology, Physics, lead author Dr. Farshad Foroudi and colleagues in the radiation oncology unit at Kingston General Hospital in Kingston, Ontario, state that their findings will facilitate long-term planning of radiation services for prostate cancer patients.
They noted that, although epidemiologists can accurately predict the future incidence of cancer, it has been more challenging to determine the proportion of such cases that will require radiotherapy, and that radiotherapy utilization rates vary widely, ranging from 20% to over 50%.
Foroudi and colleagues reviewed the literature and took into account several variables used to define indications for radiotherapy in prostate cancer: Gleason grade, clinical stage, levels of prostate-specific antigen (PSA), and status of margins and nodes, as well as symptoms, treatment history, and response to other treatment.
They documented seven scenarios for radiotherapy for the initial management of prostate cancer, and six such scenarios for radiation for either progression or recurrence. The initial scenarios were defined by risk (low, moderate, or high), status of margins and lymph nodes, history of radiotherapy, and bone metastasis. The progression or recurrent scenarios were characterized by local recurrence, spinal cord compression, regional presentation, widespread bone metastasis, progressive local disease, and bone pain symptoms.
The investigators’ review of cancer registries and other epidemiologic data showed that 61.2% of prostate cancer patients would need radiotherapy. Further, their findings showed that 32.3% of patients would require radiotherapy initially and that 29% would require radiation later in their disease.
These findings have implications for both privately funded healthcare and for publicly funded systems, as in Canada, Foroudi and colleagues reported.
"Our method provides a rational basis for the long-term planning of RT services, which has been lacking in the past," they wrote. "Market forces can be relied on to ensure a plentiful supply of (radiotherapy) for those who are able to pay for it...However, the long waiting lists for (radiotherapy) that developed in countries with publicly funded systems in the late 1980s reflect the need for much more careful planning to ensure adequate access to care."
The authors hope their approach will help ward off such problems (International Journal of Radiation Oncology, Biology, Physics, January 1, 2003, Vol.55:1, pp.51-63). The group's long-term goal is to estimate the need for radiotherapy in a given North American cancer population and develop a model that can be adopted for the needs of any community.
By Paula MoyerAuntMinnie.com contributing writer
January 27, 2003
Related Reading
PET/CT preferred as whole-body scan for cancer detection, December 6, 2002
Combined PET and MRI distinguish necrosis from tumor recurrence, October 29, 2002
In-line PET-CT system improves cancer diagnosis, October 10, 2002
FDG-PET results keep colorectal cancer patients out of the OR, May 7, 2002
Copyright © 2003 AuntMinnie.com