The Access to Medical Imaging Coalition (AMIC) is asking the Medicare Payment Advisory Commission (MedPAC) to consider the ways in which cutting physician payments could affect access to healthcare and patient outcomes.
In a letter to MedPAC, AMIC cited a study in the December 2011 issue of Health Affairs on dual energy x-ray absorptiometry (DEXA) screenings for osteoporosis that illustrated the correlation between inadequate Medicare reimbursement and adverse patient outcomes.
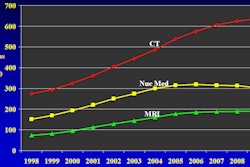
The peer-reviewed study found that DEXA testing in all Medicare Part B settings plateaued in 2007-2009 after the Deficit Reduction Act of 2005 and regulations reduced Part B imaging payments. The cuts followed a decade of growth in the use of DEXA to detect osteoporosis.
According to the study, 800,000 fewer tests than expected were performed for Medicare beneficiaries during those years. The tests may have prevented approximately 12,000 fractures and associated healthcare costs.
In a statement, Tim Trysla, AMIC's executive director, said the study demonstrates the "very real impact" of Medicare payment cuts on the health and safety of patients.