Brain SPECT for the Detection of a Seizure focus:
Partial Complex Seizures/Temporal Lobe Epilepsy:
Epilepsy is one of the most prevalent neurological disorders- affecting about 1% of the general population [10]. Seizures can be classified as either partial (focal) or generalized [2]. Partial seizures originate in a given area of the brain and can be divided into simple (with no impairment of consciousness) and complex (with impairment of consciousness) [10]. Both simple and complex partial seizures may be preceded by sensations such as smells, tingling, or buzzing [2]. About 10-20% of patients with partial complex seizures have inadequate control on medical treatment [10]. Patients unresponsive to anti-convulsant therapy may be surgical candidates which can render the patient seizure free [2]. Scalp EEG often fails to accurately localize the seizure focus and although depth EEG is much more accurate, it is also extremely invasive and suffers from regional under sampling. Most partial complex seizures originate in the temporal lobe. The most common pathologic finding in these patients is mesial temporal sclerosis which is thought to represent a gliotic scar. Excision of this focus can lead to elimination of the seizures or significantly improved pharmacologic control in 80% of patients. CT and MRI have low sensitivity for seizure foci detection, 17% and 34% respectively. The role of brain SPECT is to localize the seizure focus [2].
Ictal Imaging:
The ictal exam requires that the patient be placed in a special room with continuous video and EEG monitoring. The patients medication is usually tapered off or discontinued to increase the likelihood of a seizure episode [2]. The tracer to be used is placed by the patients bedside and is already labeled. During the ictal phase of a complex partial seizure, there is typically hyperperfusion of the mesial or lateral aspects of the affected temporal lobe. Tc99m-HMPAO of Tc-99m ECD injected during the ictal state or in the immediate post-ictal period (within 30 to 60 seconds) will show a focal area increased activity (hypermetabolic region) at the seizure focus in 80 to 100% of patients. Crossed cerebellar hyperperfusion can also be identified in 75% of patients [10]. Ipsilateral or diffuse cerebellar hyperperfusion may also be seen [11]. Ipsilateral basal ganglia hyperperfusion is also common [11]. The injection should be performed before the seizure becomes generalized as identification of the seizure focus may not be possible should this occur [10]. Ictal SPECT studies have reported sensitivities between 81 to 93% [5,11]. The positive predictive value of SPECT imaging for localizing a unilateral seizure focus can be as high as 97% (when the tracer was injected immediately after the seizure) [9].
Early post-ictal scans (injection within minutes [1 to 10 minutes] following seizure termination) can demonstrate mesial hyperperfusion and/or lateral temporal hypoperfusion on the side of the seizure focus. Such abnormalities are seen in about 70% of cases. The mesial hyperperfusion often has a crescent appearance and rarely persists for more than 6 to 8 minutes following the seizure, but can disappear as rapidly as 1 to 2 minutes. The associated lateral hypoperfusion often persists for longer periods of time (up to 20 minutes) and can be seen bilaterally, although it will be more pronounced on the side of the seizure focus.
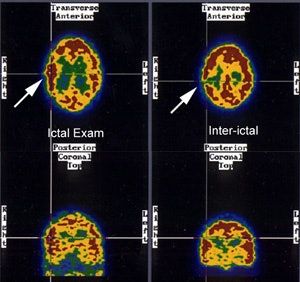
Conventional image interpretation suffers from several limitations [11]. Side-by-side visual analysis is required to identify the seizure focus. The interpreting physician must visually account for slight differences in the patients head and image slice location when evaluating the exams [11]. Computer-aided co-registration subtraction imaging of the ictal and inter-ictal exams can improve the sensitivity of SPECT imaging in localizing the seizure focus [11].
Inter-ictal Imaging:
Following the seizure, there is relatively rapid progression (generally within 20 minutes) to a hypoperfused state which persists throughout the inter-ictal phase. Inter-ictal (seizure free) SPECT studies will demonstrate an area of diminished tracer activity at the seizure focus in up to 50% of patients. Inter-ictal PET FDG studies demonstrate a focal area of hypometabolism in 60 to 70% of patients with normal MRI's [1,2,3]. The area of hypometabolism is often much larger than the actual area of structural abnormality. It is difficult to assess the relationship of medical therapy to the finding of inter-ictal hypoperfusion. Anticonvulsants, especially phenytoin and phenobarbital, are known to reduce cerebral and cerebellar metabolism [4]. Up to 10% of patients may have a hypermetabolic focus identified on inter-ictal exams (which may appear hypometabolic on subsequent exams) [10]. Hypoperfusion of the ipsilateral thalamus can be seen in 26% of interictal exams [10].
Both HMPAO and ECD are equivalent for localization of a seizure focus [10]. The sensitivity for localization of the ictus site using inter-ictal SPECT scanning ranges from 40 to 66%, which is less sensitive than post-ictal (70%) or ictal (80-90%) SPECT, and inter-ictal PET FDG (70%) imaging. Incorrect localization is seen in 5 to 15% of cases. This may occur because rCBF in the seizure region is increased from its interictal value if the tracer is injected after subclinical seizure or during a time when there is an elevation in interictal spiking. The contralateral temporal lobe will then appear to have lower rCBF. Prognostically, patients with normal SPECT findings in the face of a localizing EEG are at a higher risk for a poor surgical outcome [4]. A combination of hypoperfusion in the inetrictal study followed by hyperperfusion in the same region on the ictal exam has absolute specificity [10].
|
Seizure focus: Ictal SPECT perfusion exam demonstrates a hyperperfused (metabolic) area in the right temporo-parietal region which corresponds to a hypoperfused region on the inter-ictal exam. (Click image to enlarge) |
|
|
The benzodiazepine (BN) receptor is a marker of the GABA-BN complex which is believed
to be the main mediator of neuronal inhibition. GABA and BN receptor antagonists have been
shown to induce seizures. C-11 flumazenil (C-11 FLU) is a benzodiazepine antagonist with
high affinity for the central type benzodiazepine receptor that forms part of the GABA
receptor. Both PET and SPECT studies have shown reduced BN receptor binding exclusively in
the epileptic focus in patients with
partial epilepsy, even when the cerebral perfusion exam is normal. [4] C-11 carfentanil
studies of patients with partial complex seizures have demonstrated increased opiate
receptor binding in the temporal lobe containing the epileptic focus (corresponding to the
area of decreased glucose utilization identified on FDG imaging).
Frontal Lobe Epilepsy:
In the evaluation of frontal lobe epilepsy, SPECT images performed following the injection of Tc99m-HMPAO during the ictal period, demonstrated a hypermetabolic/hyperperfused seizure focus in 90% of cases. Hyperperfusion of the ipsilateral basal ganglia (73%) and contralateral cerebellum (64%) were also identified. Contralateral cerebellar hyperperfusion was primarily associated with seizure foci located in the motor cortex or frontopolar regions. Inter-ictal SPECT imaging detected a hypoperfused seizure focus in only 11% of patients and therefore, interictal scanning is probably only useful in serving as a baseline exam. [3]
Status Epilepticus:
Status epilepticus is a condition in which seizures occur either continuously or so frequently that patients do not return to their baseline state between seizures. Although EEG can be very useful in the diagnosis, EEG abnormalities may be subtle or absent in these patients. In the evaluation of partial status epilepticus, ictal SPECT studies have demonstrated focal hyperperfusion in areas concordant with that suggested by EEG. In patients without status, no areas of hyperperfusion were detected. Status epilepticus produces long term changes in regional cerebral blood flow that are not evident following a single seizure. As a result of this, persistent hyperperfusion may be observed for a prolonged period of time (possible out to 6 days following the event). [7]
REFERENCES:
(1) J Nucl Med 1993; Henry T, et al. Clinical evaluation of interictal
fluoring-18-fluorodeoxyglucose PET in partial epilepsy. 34: 1892-1898
(2) J Nucl Med 1993; Newton M, et al. Ictal SPECT using technetium-99m-HMPAO: Methods for rapid preparation and optimal deployment of tracer during spontaneous seizures. 34: 666-670
(3) Neurology 1993; Harvey AS, et al. Frontal lobe epilepsy: clinical seizure characteristics and localization with ictal 99mTc-HMPAO SPECT. 43: 1966-80
(4) J Nucl Med 1994; Devous M. Editorial: The role of SPECT brain imaging in epilepsy. 35: 1094-96 (No abstract available)
(5) Radiol Clin North Am 1993; Van Heertum RL, et al. SPECT brain imaging in neurologic disease. 31: 881-907
(6) Nuclear Medicine Annual 1994; Mountz JM, et al. Brain SPECT: 1994 Update: 1-54 (p.35) (No abstract available)
(7) J Nucl Med 1994; Tatum WO, et al. Technetium-99m-HMPAO SPECT in partial status epilepticus. 35: 1087-1094
(8) J Nucl Med 2000; Lewis PJ, et al. Does performing image registration and subtraction in ictal brain SPECT help localize neocortical seizures? 41: 1619-1626
(9) J Nucl Med 2001; Catafau AM. Brain SPECT in clinical practice. Part I: Perfusion. 42: 259-271
(10) J Nucl Med 2001; Camargo EE. Brain SPECT in Neurology and Psychiatry. 42: 611-623
(11) J Nucl Med 2001; Shin WC, et al. Ictal hyperperfusion of the cerebellum and basal ganglia in temporal lobe epilepsy: SPECT subtraction with MRI coregistration. 42: 853-858