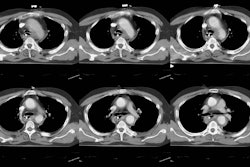
Spiral CT of acute pulmonary thromboembolism: evaluation of pleuroparenchymal abnormalities.
Johnson PT, Wechsler RJ, Salazar AM, Fisher AM, Nazarian LN, Steiner RM
PURPOSE: The goal of this work was to identify and categorize the spectrum of pulmonary parenchymal and pleural abnormalities identified by CT in patients with acute pulmonary thromboembolism (PE). METHOD: A review of interpretations from 4,715 consecutive contrast-enhanced thoracic CT studies identified 41 examinations in which the diagnosis of PE was reported. Thirty-four studies were available for review, and two radiologists confirmed intraluminal defects in 31 patients. The number of emboli were counted and localized using bronchopulmonary nomenclature. Associated parenchymal and pleural abnormalities were tabulated. RESULTS: Of the 31 patients, 13 underwent confirmatory or correlative studies including angiography, radionuclide study, or autopsy. In addition, deep venous thrombosis was confirmed by ultrasound or MRI in 13 patients. An average of 7.5 emboli per patient was detected. Pleuroparenchymal findings were as follows: Nine patients (29%) had no acute pulmonary parenchymal or pleural abnormality. In the remaining 22 patients, pleural effusion was the most common abnormality, found in 14 of 31 (45%). Ten patients (32%) had peripheral wedge-shaped parenchymal opacities suggestive of pulmonary infarction. Normally enhancing lobar atelectasis was seen in nine patients (29%). Six patients (19%) demonstrated heterogeneous parenchymal enhancement within nonaerated lung, two of whom had pathologically proven pulmonary infarct. Thirteen of 31 patients underwent high resolution CT; a typical mosaic perfusion pattern was seen in only 1 patient. CONCLUSION: Twenty-nine percent of patients with acute PE had no acute lung parenchymal abnormality on CT; thus, the absence of parenchymal abnormality on CT does not exclude PE. High resolution CT mosaic perfusion was not a common feature of acute pulmonary embolism. Regions of decreased enhancement within nonaerated lung, seen in 19%, may prove to be an indicator of pulmonary infarction; however, this is a nonspecific finding.
PMID: 10348441, UI: 99276197