Healthcare simulation can help radiology departments to understand -- and address -- safety, quality, and efficiency issues for a variety of applications, according to a presentation on August 1 at the 2021 AHRA meeting in Nashville, TN.
 Traci Foster of Texas Children's Hospital the Woodlands.
Traci Foster of Texas Children's Hospital the Woodlands.In her talk, Traci Foster of Texas Children's Hospital the Woodlands described the process of healthcare simulation and shared how the technique helped her institution to prepare for a new mobile MRI unit.
"Simulation is an invaluable tool that is gaining momentum worldwide and can be used in all aspects of healthcare -- including radiology -- to allow for safer and higher-quality care for our staff as well as for our patients," Foster said.
Simulation consists of four components:
- Preparation: Aligning the simulation with the learning objectives and goals
- Prebrief: Setting the stage and sharing the rules with the participants
- Simulation: Practicing the practice
- Postbrief: Judgement-free reflection on what happened during the simulation
Guiding principles
Simulation has several important guiding principles that are crucial to creating what is referred to as psychological safety: being able to show one's self without fear of negative consequences to self-image, status, or career, Foster said.
The basic assumption is that everyone participating is intelligent, capable, and cares about doing their best and trying to improve, she said. Confidentiality is also crucial.
"What happens in the sim stays in the sim," Foster said.
Another guiding principle is the "fiction contract," a contract between the instructor and learner(s) that implies each has to do their part to make the simulation worthwhile.
"When a gap occurs between simulated reality and actual reality, it is expected that the learner understands the goals of the simulation and behaves accordingly," Foster said.
To perform task simulations, you'll need some equipment, such as human patient simulators (i.e., high-fidelity manikins) to enable more real-life human-to-human interaction. In addition, task trainers simulate a part or an area of the body and enable repeated practice of specific procedural skills, she said.
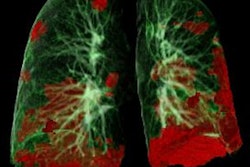
 Using simulation with a focus on assessing patient safety, Texas Children's Hospital identified latent safety threats that enabled the institution to determine their scope of sedation services in the mobile MRI unit. Image courtesy of Traci Foster.
Using simulation with a focus on assessing patient safety, Texas Children's Hospital identified latent safety threats that enabled the institution to determine their scope of sedation services in the mobile MRI unit. Image courtesy of Traci Foster.Thanks to recent software and equipment innovations, virtual-reality simulators are also gaining momentum in healthcare simulation, Foster said.
The most important part
Foster emphasized the importance of the simulation post-event debriefing. Debriefing is the process of obtaining feedback from all involved and enables the situation to be reviewed and discussed free of judgment. Debriefing can occur during and after the simulation.
The postevent debrief, which typically takes two to three times longer than the actual simulation, includes a reaction phase, an in-depth analysis, and discussion of the lessons learned. The postevent debrief is meant to obtain feedback from everyone -- including observers -- involved in the simulation and enable a review and discussion that's free of judgment, according to Foster.
Foster then shared some examples of how Texas Children's Hospital the Woodlands has utilized healthcare simulation in radiology. In October 2018, the 74-bed community hospital's radiology department sought to replace both of its 1.5- and 3-tesla MRI scanners. As both scanners were to be replaced simultaneously, a mobile MRI unit was going to be needed.
"No facility within TCH had ever utilized a mobile MRI before so we had a steep learning curve," she said.
Three different simulations were used to prepare for the unit's arrival. Performed before the mobile MRI unit even arrived, the first simulation used duct tape to outline the outside as well as the inside dimension of the mobile unit on the pavement to enable the team to get a sense of the mobile unit and space constraints, processes, and workflows, as well as to begin to identify specific roles and responsibilities, Foster said.
A second simulation was performed after the mobile unit arrived to test the flow process for an unplanned emergency for anesthesia patients in the mobile MRI. The third simulation aimed to determine if sedation could be safely performed in the mobile MRI.
Identifying safety threats
The simulations identified a number of potential latent safety threats. There was a very high-risk threat from the six-minute extraction time for moving patients from the mobile MRI to the postanesthesia care unit and a high-risk threat of the equipment and stretcher not fitting on the lift, according to Foster. She also noted a moderate risk of chairs being too big for the space.
Due to the identified safety threats, it was unanimously decided to not perform sedation in the mobile MRI, Foster said.
"This meant that all sedation inpatient MRIs would have to be done at our main campus or our other community hospital and the patient would have to be transported via ambulance, despite this decision being very costly and a big patient dissatisfier," she said. "However, because we had performed multiple simulations which focused on patient safety and quality of care, we received absolutely no pushback from administration on our decision and received nothing but support."
Simulation could have a wide range of other uses in radiology, such as managing situations like a nonresponsive patient in MRI, a contrast reaction in CT, donning and doffing personal protective equipment (PPE), and using new equipment such as a Hoyer patient lift.
"The list is endless," Foster said.