Multidisciplinary work is key to modern medicine, and one example of this is the smooth cooperation between radiology and gastroenterology. Imaging has become central to the detection, staging, and follow-up of many diseases, including colorectal cancer, one of the most widespread carcinomas worldwide. Technical refinements such as the recent introduction of virtual colonoscopy using CT have notably improved its early diagnosis. Experts discussed how to further improve results during the ESR Meets Gastroenterologists session Friday at ECR.
Optical colonoscopy (OC) is the gold standard for the detection and post-treatment follow-up of colorectal cancer. Its practice enables biopsy and treatment of polyps during the same session. But virtual colonoscopy (VC) offers specific advantages, such as the possibility of reviewing images repeatedly. VC is more comfortable than OC, and it enables the imaging of patients who cannot undergo a complete examination with colonoscopy due to stenotic changes or other technical difficulties. Depending on the specific case, VC can also be a good alternative in the case of low prevalence.
"Everybody agrees that incomplete OC is an excellent indication for VC, as well as individual detection in cases of low anticipated prevalence," said ECR 2011 President Dr. Yves Menu, chairman of the department of radiology of Saint Antoine Hospital in Paris.

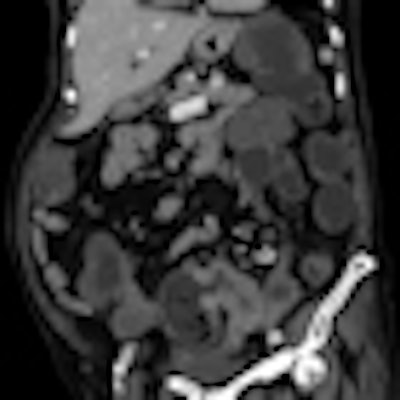
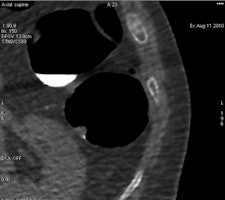
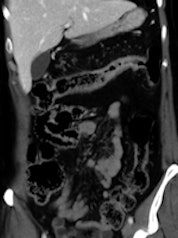 Left: Elderly patient presenting with low-grade bowel obstruction. Optical colonoscopy was denied due to patient's condition, and a CT with water enema was performed in order to detect a large lesion. This was the case because the patient had an almost occlusive cancer of the sigmoid. Right: Crohn's disease involving the transverse colon, with wall thickening and hyperhemia of the colonic vessels. All images courtesy of Dr. Yves Menu.
Left: Elderly patient presenting with low-grade bowel obstruction. Optical colonoscopy was denied due to patient's condition, and a CT with water enema was performed in order to detect a large lesion. This was the case because the patient had an almost occlusive cancer of the sigmoid. Right: Crohn's disease involving the transverse colon, with wall thickening and hyperhemia of the colonic vessels. All images courtesy of Dr. Yves Menu.The modalities appear to be becoming increasingly complementary. Follow-up programs can also include VC in association with OC. In patients requiring prolonged follow-up, both methods can be interleaved for the detection of polyps or recurrence.
However, areas of doubt remain concerning false positives in the case of fecal occult blood tests.
"In a patient with a positive fecal occult blood test, knowing the high rate of false positives, we lack evidence today to decide whether VC is a valuable step or if we should proceed immediately to OC. Some studies are ongoing and might provide us with some guidelines in the near future," Menu said.
 Acute ileal involvement by Crohn's disease, with wall thickening and mucosal enhancement.
Acute ileal involvement by Crohn's disease, with wall thickening and mucosal enhancement.
Technical advances in MRI have improved the staging of rectal cancer, especially in the prediction of local invasion. MRI is crucial when discussing a potential indication for neoadjuvant radiochemotherapy, and it also provides useful information when deciding surgical strategy. "In this indication, MRI is very complementary to rectal endosonography," he said.
Surgery is still the main treatment option, and surgical techniques have been considerably improved. In parallel, the use of radiation and cytostatics also has increased chances of survival.
National screening programs for the early detection of colorectal cancer also could improve outcome. But although the European Union has recommended their launch in all countries, most of them still do not have a well-functioning program, mainly because of a lack of awareness from politicians and healthcare officers, believes Dr. Rolf Hultcrantz, a professor of gastroenterology and hepatology at Karolinska University Hospital, and president of the United European Gastroenterology Federation (UEGF).
"There are screening programs in some countries, such as England, Finland, Italy, and a part of Sweden. In other countries, screening is available but not actively offered to the whole population. There may be a problem with the availability of colonoscopists across the EU, but the main problem I think is politicians' awareness and willingness to allocate resources for this purpose," he said.
Many other gastroenterological pathologies require imaging for detection and evaluation. Ultrasonography is the first step when liver, pancreatic, or biliary disease is suspected. In inflammatory bowel diseases, CT and more recently MRI have proved to be valuable tools for detecting and staging the disease, as well as for monitoring treatment.
"Overall, gastroenterology is a specialty where imaging is dramatically important, as well as biology, but always in association with clinical examination. The number of patients who require treatment monitoring is certainly increasing and imaging is a pillar in their surveillance," Menu said.
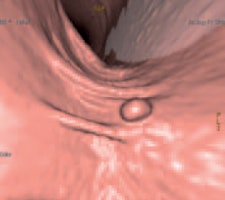 ColoVirt 2D and 3D show the same image of a small (7 mm) sessile polyp of the descending colon.
ColoVirt 2D and 3D show the same image of a small (7 mm) sessile polyp of the descending colon.Recent technical developments in radiology have improved both the detection and characterization of diseases. Advances are still ongoing, for instance with PET/CT in the management of cancer, as imaging gears up toward depicting function and metabolism, and enabling structure analysis. Striking evidence for this is the management of diffuse liver diseases, according to the ECR 2011 president.
Several noninvasive methods, such as ultrasound/MR elastography, diffusion-weighted MRI, as well as biological tests, provide an excellent view of liver fibrosis. Fatty liver disease and iron overload also can be quantified noninvasively. A significant number of liver biopsies can now be avoided, to the greatest benefit of patients," he explained.
Radiologists are also gathering more and more information from inflammatory bowel disease and digestive oncology in general.
The challenge faced by gastroenterological imaging today is to determine as fast as possible the optimal strategies for detection, characterization, and treatment monitoring. This goal, along with the financial constraints in many institutions, means immediate improvements in efficiency are necessary, as well as increased cooperation with other disciplines.
"We should recognize that the future of medicine is to improve prevention and personalization. This will not be possible unless all organizations cooperate closely, because it concerns not only the gastroenterologist and the radiologist but also other scientists like biologists, epidemiologists, and many more," Menu said.
Fortunately, things are running smoothly between gastroenterologists and radiologists.
"Our collaboration is excellent. The basis for all decision-making in gastroenterology and many other clinical specialties is multidisciplinarity, and in this process radiologists are a very important part," Hultcrantz said.
"Although we have potential competition between endoscopy and imaging, for instance with the development of endosonography, small-bowel imaging versus capsule endoscopy, and virtual versus optical colonoscopy, the relationship between gastroenterologists and radiologists has always been more a scientific debate rather than a turf battle. Although the discussions are sometimes passionate, neither the gastroenterologist nor the radiologist would ever fight against scientific evidence," Menu said.
The participation of the UEGF in the "ESR Meets" initiative this year will certainly provide more visibility for this successful cooperation.
Originally published in ECR Today March 4, 2011.
Copyright © 2011 European Society of Radiology