In women with dense breasts, mammography's sensitivity can be as low as 60%. In other words, up to 60% of breast cancers can be misdiagnosed in these women. Clearly, something must be done, and something is: Today, presenters are showcasing tools for quantification and will explain how high breast density may lead to changes in imaging strategies.
First up, Dr. Fiona Gilbert from the department of radiology at the University of Cambridge in the U.K. will address the "problem child" modality radiologists must deal with on a regular basis: mammography. ECR delegates will learn about the definition of dense breasts and what they look like on mammography. In addition, they will understand the different methods to measure breast density on mammography and analyze details that can be associated with abnormalities in dense tissues.
Breast density can be measured using different techniques such as the Boyd and Cumulus techniques, and there are different scoring systems for assessing the amount of breast density on mammography, particularly the BI-RADS systems, and the Royal College of Radiologists (RCR) breast group system. In addition, quantitative methods are becoming available, such as Volpara and Quantra software.
"The reason these techniques are important is because firstly, and most importantly, an assessment of breast density on mammography gives the reader an indication of sensitivity of the mammogram to detecting breast cancer. BI-RADS 4, BI-RADS D, or 'dense breast' in the U.K., implies that the sensitivity is reduced compared with someone who has fatty breasts or BI-RADS A or I," she said. "There is a masking effect because of dense breast tissue, reducing the likelihood of detecting breast cancer."
Thus, knowing breast density provides essential information. Delegates will be particularly keen in Gilbert's talk as she'll go through the different ways of measuring breast density, addressing how reliable they are.
"Everyone encounters dense breasts, so it will be relevant. Also, there is increasing concern about whether something additional should be offered to women who have dense breasts on mammography," she said.
However, sometimes additional imaging techniques need to be performed, and that's where the other presentations come in.
Dr. Luis Pina Insausti from the department of radiology at Clinica Universitaria de Navarra in Pamplona, Spain, will discuss ultrasound and dense breasts. Ultrasound can detect additional breast cancers in dense breasts after negative mammography, increasing the detection rate of breast cancer by up to 37%.
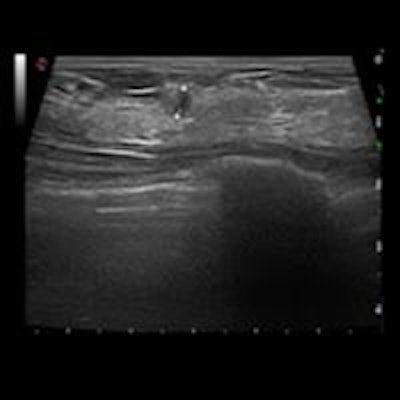
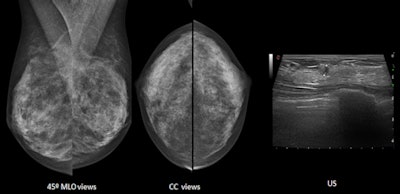 Both mammographic views (mediolateral oblique and craniocaudal) are normal on these heterogeneously dense breasts. Ultrasound detects a 5-mm invasive ductal carcinoma. Images courtesy of Dr. Luis Pina Insausti.
Both mammographic views (mediolateral oblique and craniocaudal) are normal on these heterogeneously dense breasts. Ultrasound detects a 5-mm invasive ductal carcinoma. Images courtesy of Dr. Luis Pina Insausti.Handheld ultrasound can only be performed for selected patients in a clinical setting, and it cannot be offered in a screening setting for all patients, he explained. Automated breast ultrasound, on the other hand, can play a central role in increasing the detection of additional cancers in the screening of dense breasts; the technologist performs the examination and later the radiologist reads the images.
"Breast ultrasound is an excellent tool that can significantly increase the sensitivity of mammography," Insausti said.
The American College of Radiology BI-RADS lexicon describes three patterns for ultrasound breast composition: homogeneous echotexture -- fat, homogeneous echotexture -- fibroglandular, and heterogeneous echotexture. The patterns have similarities with mammographic density patterns (dense mammographic patterns can be seen as homogenous echotexture -- fibroglandular and heterogeneous echotexture patterns).
"Due to the fact that most benign and malignant lesions are usually seen as hypoechoic masses, these lesions are better detected on homogeneous echotexture -- fibroglandular than on the other patterns," he added.
Moreover, there are other less obvious factors that can influence the detection of lesions with ultrasound: volume of the breast (attenuation of ultrasound in large-sized breasts can decrease the sensitivity of ultrasound), localization of the lesion (worse visualization in deeply or superficially located lesions, or lesions located behind the nipple or scars), and atypical appearance of some breast cancers (hyper- or isoechoic cancers, subtle distortions, etc.).
Rounding out the session, Dr. Pascal Baltzer from the department of radiology at the Medical University of Vienna, will discuss breast density in MRI, which is considered an ambiguous term.
"It mainly refers to the amount of fibroglandular tissue that should be assessed and categorized according to the BI-RADS lexicon," he said.
As known from mammography studies, the amount of fibroglandular tissue is an independent risk factor for development of breast cancer, and MRI may assess this risk factor in a volumetric, 3D manner.
"This is why some authors consider MRI assessment of breast density superior to mammographic assessment," Baltzer noted.
After contrast agent administration, breast parenchyma can show various levels of enhancement, referred to as background parenchymal enhancement, which is referred to as "MRI breast density" by some authors. This connection is based on the assumption that a marked background parenchymal enhancement may decrease the diagnostic performance of breast MRI in analogy to the amount of fibroglandular breast tissue in mammography.
Baltzer's talk will deal with both aspects of breast density and provide delegates with evidence-based clinical knowledge. Following his presentation, there will be a panel discussion on how to overcome the dense breast in screening.
Originally published in ECR Today on 4 March 2016.
Copyright © 2016 European Society of Radiology