An unexpected consequence of PACS is that radiologists are increasingly sidelined by referring physicians to the extent that if a patient comes into the emergency room with a suspected fracture, the physician can look at the images to make a diagnosis and may not even read the radiologist's report, according to Dr. Johan Van Goethem from the department of neuroradiology at Antwerp University Hospital in Belgium.
This problem is confounded as physicians grow more specialized. In their areas of special interest, they can increasingly read images with equivalent skills to a radiologist.
"Many radiologists don't see it coming yet, but our profession is in real danger if we don't act swiftly in the coming years to change the way we work," he said.
Moreover, although radiologists have an active role in many multidisciplinary teams, some referring physicians don't appreciate the work they do. Also, the public and media are often unaware of the work of radiologists, believing that radiologists are mere technicians who take images to be interpreted by a referring physician.
"We need to interact with the public and press to highlight our function," Van Goethem urged. "We're weakening our position if we don't have them on our side."
Radiologists must interact more with patients rather than sitting in a darkened room, and they must also place themselves inside the clinical loop by discussing more cases with referring physicians and becoming more active members of multidisciplinary teams, he continued.
An important future role of radiologists might be as a gatekeeper. This may include screening referrals for the appropriateness of the technique and limiting access to examinations. Here the benefit is financial, and Van Goethem explains that if the same physician diagnoses and prescribes, therapy costs rise exponentially. In spine imaging, for example, radiologists recommend no imaging for acute lower back pain without leg pain for the first eight weeks because it doesn't aid therapy, and this reduces both costs and patient exposure to ionizing radiation.
Additionally, he recommends that radiologists focus on examinations, such as MRI today and spectral imaging in CT in the future, that referring physicians find too complex to report or interpret.
Radiologists should also superspecialize to gain the respect of referring physicians, Van Goethem believes. They should be aware, for example, of the techniques used by orthopedic surgeons, the complications that are possible, and what both normal and abnormal postoperative imaging look like. "Otherwise you're placing yourself out of the game and radiologists aren't necessary anymore," he warned.
During today's session, ECR delegates will hear about other challenges to the profession and how they can respond. Dr. Gabriel Krestin, PhD, chairman of radiology and nuclear medicine at the Erasmus Medical Centre in Rotterdam, the Netherlands, thinks the training of radiologists needs to adapt to prepare the next generation for future changes in the profession.
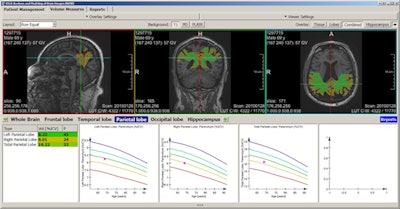 The fully automated segmentation and quantification of different brain regions based on a machine learning algorithm. Software enables the identification of patients at risk of developing dementia long before symptoms of cognitive impairment are apparent. Images courtesy of Dr. Gabriel Krestin, PhD.
The fully automated segmentation and quantification of different brain regions based on a machine learning algorithm. Software enables the identification of patients at risk of developing dementia long before symptoms of cognitive impairment are apparent. Images courtesy of Dr. Gabriel Krestin, PhD."The radiologists who will be practicing in 20 to 30 years' time will need to understand more about the molecular basis of diseases, understand the power of computers and artificial intelligence, and deal with big data, and data analytics," he said. "This is something we need to introduce as fast as possible into our education."
Deep machine learning will make some aspects of the job easier, but it also raises some philosophical questions. For example, if computers can analyze the raw data underlying MRI and CT images, do radiologists need images at all?
Krestin suggests that the future role of radiologists will be more about consulting with clinicians in a multidisciplinary team, handling data, and answering their questions. To perform this role, radiologists would need to change their daily practice, moving from describing images to interpreting and integrating information from blood tests, imaging, and genetic sequencing.
Other speakers in the session will talk about turf battles resulting from more cardiologists, neurologists, and other physicians reporting CT or MRI examinations. Who should report examinations presents a different type of challenge to the profession. There will also be a talk about how SWOT (strengths, weaknesses, opportunities, and threats) analysis can help radiologists understand their strengths as a profession and how to focus on these.
Originally published in ECR Today on 4 March 2017.
Copyright © 2017 European Society of Radiology