Swedish researchers report positive results using ultrasound for the diagnosis and treatment of breast abscesses in lactating women. Dr. Dieter Ulitzsch and colleagues from Danderyds Hospital in Stockholm examined 108 women with clinically suspected breast abscesses over a three-year period at their institution.
"Breast abscess is a rare, but potentially serious, complication of mastitis. At Danderyds, ultrasound guidance has been used successfully for many years in treating breast abscess," said Dr. Richard A. Carlson in a presentation at the 2002 RSNA meeting in Chicago. "It was decided to report and study this institution’s experience, specifically in lactating women." Carlson, a study co-author, is with Suburban Radiologic Consultants in Edina, MN.
The patient population included all lactating women who were referred to the Danderyds breast center because of clinical suspicions of abscess. The average time of diagnosis following delivery was five and a half weeks, Carlson said.
Among 108 women, 56 abscesses were discovered on ultrasound. Six of the women in this study had multiple -- up to four -- abscesses. The ultrasound findings associated with mastitis included a hyperechoic parenchyma, increased vascularity, increased fat echogenicity, skin thickening, distended lymphatic channels, and reactive lymph nodes, Carlson said.
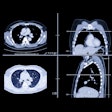
 |
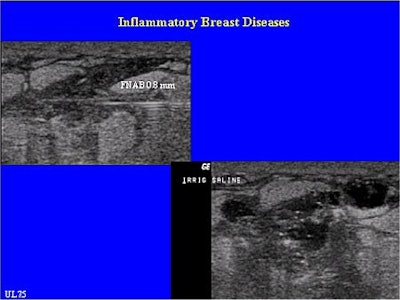
| These ultrasound images are from a patient with a mature abscess and no signs of surrounding mastitis. The top scan depicts the mature puerperal abscess; the bottom image shows the reactive axillary lymph node. |
"If ultrasound showed evidence of an abscess, diagnosis was confirmed by needle puncture and the abscess was treated by ultrasound-guided drainage," he added.
"The lesion was punctured not only to confirm the diagnosis, but to obtain material for culture and to determine puss viscosity. Once needle puncture confirmed the diagnosis, ultrasound-guided drainage was performed in one of two ways determined by size. Smaller abscesses were drained by needle aspiration alone, whereas catheter placement was used for larger abscesses."
Needle aspiration was performed in 23 cases; the mean size of the abscesses was 2.2 cm. The procedure involved completely aspirating and flushing the cavity with saline using 14-21 gauge needles. The patient returned for follow-up visits and re-aspiration, if necessary, until the sonographic exam showed that the lesion was completely gone. More than half of these cases required only one round of aspiration, Carlson explained.
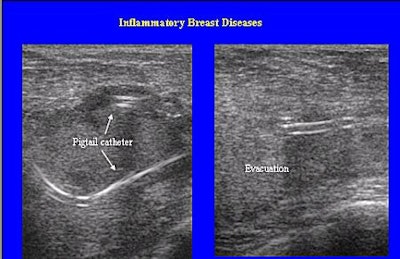 |
| A woman with a catheter in place. Note that the catheter is placed away from the nipple in order to allow for breast-feeding. |
For the 33 abscesses that were larger than 3 cm, catheter drainage was done using percutaneous catheter placement.
"After generous local anesthetic, a pigtail catheter, 6-8 French, was placed using the Trocar technique. Catheter size was based on puss viscosity. The catheter was irrigated several times until the return aspirate was clear. The patient was instructed to irrigate the catheter three times a day at home. She returned for follow-up visits every 2-3 days until the cavity was virtually gone, at which time the catheter could be removed," Carlson said.
 |
This patient has a very immature abscess with many small cavities in the seriously inflammed tissue and surrounding mastitis. These cases are often difficult to treat and repeated aspirations are required. Images courtesy of Dr. Dieter Ulitzsch.
 |
Some of the catheter placement techniques that the team recommended are to avoid going through inflamed tissue as well as keeping the catheter away from the periaeolar area so that breast-feeding can continue. Most women do continue breast-feeding with the catheter in place, Carlson said.
The ultrasound-guided treatment was deemed successful in 55 cases; only one patient required surgical intervention due to abscess recurrence, which was caused by milk leaking along the catheter. As a result, the catheter had to be removed prematurely.
Carlson advised that "if there is milk in the aspirate, or leaking along the catheter, it’s important to leave the catheter in place until that ceases to avoid abscess recurrence."
Ultrasound detection and ultrasound-guided treatment is now standard protocol at Danderyds Hospital, Ulitzsch wrote in an e-mail to AuntMinnie.com.
"No surgical incision or surgical operation in puerperal abscesses has been performed for at least 5 years," he wrote. "The number of treated abscesses increased (in 2002), mainly due to an increased number of deliveries. In 2002 we had more than 6,900 deliveries at our hospital...and about 42 successfully treated abscesses in 33 women."
Ulitzsch said future research would focus on the cost effectiveness of ultrasound-guided procedures for abscesses versus surgery. Some of the costs associated with the procedure include local anesthetics, saline solution, needles, and the presence of 1-2 radiographers plus a radiologist. Anecdotally, Ulitzsch said than ultrasound-guided treatment is less expensive that surgery. "The main costs beside salary is the price of the catheter (about $80-$90 U.S.)," he wrote.
By Shalmali PalAuntMinnie.com staff writer
January 28, 2003
Related Reading
Ultrasound separates galactoceles from simple cysts, April 9, 2002
Copyright © 2003 AuntMinnie.com