CSF Flow Studies:
CSF flow studies are performed using either In-111 (DTPA) or Tc99mDTPA. Indications for the exam include suspected normal pressure hydrocephalus, occult CSF rhinorrhea/otorrhea, and ventricular shunt evaluation.
Radionuclide Shunt Scintigram:
CSF shunts have a high failure rate which can reach as high as
50% in the two years following placement [7]. In a young shunted
child, it can be very difficult to differentiate
the prodrome of a
viral illness (headache, irritability, nausea, and vomiting) from
a
shunt malfunction-
especially if the patient's CT scan appears stable. In adults, the
site of VP shunt obstruction is nearly always in the distal
catheter, while in pediatric patients obstruction of the proximal
catheter is the cause in more than 50% of shunt failures [7].
. Radionuclide
shuntograms have been used
as an adjunct to aid in evaluation of shunt malfunction.
Shunt complications include:
? Ventricular catheter blockage (most common) - malfunction of the ventriculoperitoneal shunt occurs in about 25-35% of patients at one year and 70-80% of patients require at least one shunt revsion at some point [5].
? CSF loculation at the catheter tip: The lesion occurs secondary to adhesions and results in enlarging abdominal mass (CSFoma). This is an unusual complication occuring in less than 1.0-4.5% of patients [5]. Scintigraphic findings include focal pooling of tracer in the abdomen. To treat, the shunt is externalized, antibiotics instituted, and the collection should reabsorb on its own.
? Infection: Meningitis, ependymitis, abscess. The incidence of shunt infection is between 5-47% and about 70% of shunt infections occur within 2 months of placement [5]. The most common organism is S. aureus [5].
? Subdural hematoma: Bridging veins in the subdural space may be torn with rapid decompression of hydrocephalus. This is generally a bilateral phenomenon.
? Craniosynostosis
? Aqueductal stenosis: Probably due to inflammation and results in non-communicating hydrocephalus.
? Thromboembolism: With cardiac atrial shunts
Any process that interferes with CSF flow from the shunt
reservoir will result in absent or diminished passage of tracer
through the shunt components [7]. Nuclear medicine CSF shunt
studies evaluate not only the integrity of the proximal and distal
catheters, but also the valve as well [7]. The valve is designed
to open and close at specific pressures and the valve may fail to
function properly due to valve obstruction from debris or blood
products or valve failure [7].
Tc99m-DTPA or Tc99m-pertechnetate are the commonly
used agents [7]. In-111
DTPA (0.15-0.2 mCi) can be used when longer imaging times may be
required.
Patients are placed in a supine position for approximately 15
minutes. A small volume
(0.1mL to 1 mL) of the agent is injected into the shunt reservoir
and reflux of
the agent into the
ventricle is attempted [7]. Once the shunt reservoir is accessed,
if there is no spontaneous flow of CSF into the needle hub, the
patient may be asked to perform a Valsalva maneuver [7]. If that
does not work, one can use a 3 mL syringe to gently aspirate some
CSF into the needle hub to confirm successful access of the
reservoir [7]. It is important not to withdraw significant
amounts of CSF prior
to the injection as this may affect CSF flow and produce spurious
results. Once CSF fills the needle hub, CSF opening pressure is
measured [7]. In healthy individuals, values for intracranial
openning pressures vary with age and range from 2 cm H2O
in neonates to 15 cm H2O or less in adolescents
[7]. Absent or sluggish CSF flow associated with a
nonmeasurable or very low opening pressure is strongly correlated
with proximal catheter obstruction or valve failure/malfunciton
[7]. In complete obstruction of the proximal catheter, no CSF
fluid is seen in the needle hub [7]. An inability to aspirate CSF
fluid with a 3 mL syringe has a sensitivity of 62% for proximal
shunt obstruction, but false positive findings can be seen in
patients with normally functioning shunts who have small
ventricles on CT [7]. Sluggish CSF flow associated with an
unequivocal high CSF opening pressure (>20 cm H2O)
signifies shunt dysfunction involving the components distal to the
reservoir (valve failure/malfunction or obstruction of the distal
catheter/complications in the drainage compartment [7].
Once the tracer has been instilled into the reservoir and has
flowed into the valve, the combination of the reservoir and valve
should produce a figure 8 (bilobed) appearance to the tracer
activity at the injection site [7].
Following injection of the tracer, anterior dynamic images of the
head and neck are obtained at 10 second intervals for a total of 5
minutes [7]. Anterior static images of the head and neck, followed
by static images of the chest and abdomen are subsequently
obtained [7].
Spontaneous or induced intraventricular reflux of the tracer is highly indicative of patency of the proximal shunt catheter [7]. Activity should rapidly clear from the ventricle and should pass through the shunt tubing into the abdomen (normal flow from the injection site through the shunt to the abdomen is typically observed by 10-20 minutes after injection [6,7]). If there is lack of visualization of tracer activity in the drainage compartment, maneuvers such as having the patient sit, stand, or be held upright for 10-15 minutes can be performed before repeating static images [7]. The maneuvers evaluate for the presence of CSF flow through the patent shunt components that are facilitated by gravity drainage [7]. Failure to observe transit of activity through the shunt system despite upright positioning of the patient and pumping of the shunt reservoir is suggestive of shunt obstruction [6].
A reservoir emptying T1/2 can be determined and should typically
be less than 10 minutes [7]. One study suggested an emptying T1/2
of 8.7 minutes more more correctly classified 87% of patients
requiring shunt revision [7]. A combination of tracer reflux into
the ventricle, a CSF opening pressure of 5 cm H2O or
less (or appropriate for the patient's valve pressure setting and
typically < 10-15 cm H2O), an emptying T1/2 of less
than 10 minutes (typically less than 5-7.5 minutes with a downward
slope), with normal transit to the abdomen (transit time 15-20
minutes) and distribution in the peritoneum are all components of
a normal exam [7]. Using stringently defined criteria, the exam
can have a sensitivity of 87.5%, a specificity of 51.4%, a PPV of
39.2%, and a NPV of 92% [7]. A T1/2 of less than 2-3 minutes is
suspicious for over-drainage [7].
Free spillage of activity into the peritoneal cavity should be visualized to exclude an obstructed or localized fluid collection at the distal shunt tip [6]. Images over the abdomen should demonstrate free dispersion of the tracer throughout the peritoneal cavity. Repositioning the patient several times in the right and left decubitus position may be useful to demonstrate free movement of activity [6]. Renal and bladder activity will be seen as a result of peritoneal absorption of the tracer.
For ventriculoatrial shunts, the shunt catheter should be
visualized
to the level of the right atrium, and activity should be seen in
the
kidneys and urinary bladder [6].
False positive
findings of shunt obstruction can occur if the tracer is injected
into the soft tissues adjacent to the shunt [6]. Extravasated
tracer will have a more rounded, less well defined configuration
[7]. Tracer extravasation is also indicated by the presence of
early systemic tracer activity with visualization of the thyroid
gland, blood pool, and stomach on early 5 minute images [7].
However, early systemic activity can be seen in patients with
ventriuloatrial shunts, so it is important to know the type of
shunt the patient has [7].
Delayed, but complete
transit of activity through the shunt system is more difficult to
interpret and may be due to a partial obstruction, a decreased
driving
pressure for CSF flow, or shunt valves set to open at
inappropriately
high pressures [6]. Withdrawal of CSF before or during the
radiotracer
injection may also simulate obstruction by decreasing CSF pressure
in
the shunt system below the pressure required to trigger valve
openning
[6].
The significance of the results of the examination are highly variable. Although the absence of ventricular reflux is a highly reliable indicator of proximal obstruction, a misdiagnosis rate of between 25-40% has been reported. Nearly one-third of patients with an abnormal examination may improve without surgical intervention possibly reflective of transient shunt obstruction. A false negative rate of 14% (normal study with evidence of obstruction at surgery) has been noted. [1]
Radionuclide Cisternography
For the exam 250-500 uCi of In-111-DTPA is given intrathecally (Tc99m-DTPA may be adequate in children who have more rapid transit of the CSF if imaging will not be required beyond 24 hours). In adults activity is normally seen at the basal cisterns between 1 and 6 hours after injection. Tracer activity should be at the frontal poles, interhemispheric, and Sylvian fissures by 2 to 6 hours- producing a "Neptune's trident" appearance. Activity should be at the cerebral convexities by 12 to 24 hours (no later than 48 hours) and the arachnoid villi in the sagittal sinus by 24 hours. There should be no or only minimal lateral ventricular activity seen since physiologic flow is in the opposite direction. Ventricular activity may be noted transiently in older patients between 12 and 24 hours.
In young children tracer activity will reach the basilar cisterns in 30 minutes. Retrograde filling of the ventricular system is most likely to occur between 1 and 4 hours following injection.
Normal Pressure Hydrocephalus (NPH):
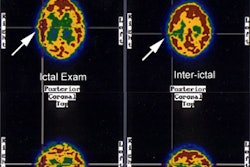
NPH is characterized by the clinical triad of mental status changes, incontinence, and ataxia, with hydrocephalus and normal CSF pressures. The scintigraphic examination demonstrates a slow ascent over the convexities with little activity seen over the vertex. Ventricular reflux with delayed clearance of ventricular activity is also seen. Late intracerebral activity can be seen and is secondary to transependymal uptake of the tracer. Surgical shunting of CSF can potentially reverse this progressive disorder. Correlation with a positive examination and benefit from shunting is poor.
Perfusion SPECT imaging in patients with NPH can demonstrate a variety of perfusion abnormalities [2,3]. Pre-operative exams have been reported to show diffusely decreased cerebral blood flow, focal abnormalities (particularly in the frontal lobes), and other perfusion defects without a specific pattern [3]. Perfusion defects can improve after shunting and correlate with clinical improvement [2,3].
|
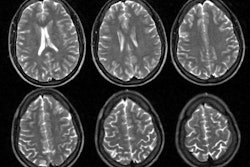
Normal Pressure Hydrocephalus: A CSF examination using In-111 DPTA is shown below. The 24 hour image demonstrates ventricular acitivity and persistent activity in the basal cisterns without evidence of activity over the convexities. Ventricular activity persists on the 48 hour exam. Some transependymal intracerebral activity is also suggested on the later images. The CT scan demonstrates the characteristic findings in NPH with ventriculomegaly out of proportion to sulcal atrophy (Click CT for additional images). |
|
|
Ventriculomegaly secondary to atrophy (Hydrocephalus ex-vacuo):
Transient ventricular activity may be identified, typically cleared by 24-48 hours.
Communicating Hydrocephalus:
Refers to an extraventricular obstruction in the basal cisterns, cerebral convexities, or arachnoid villi. Etiologies include a previous subarachnoid hemorrhage, meningitis, or leptomeningeal carcinomatosis. On scintigraphy, there is delayed flow over the convexities and reflux of activity into the ventricles with marked, persistent ventricular activity out to 72 hours. Differentiation from NPH is based upon clinical findings.
CSF Leak Study:
CSF leaks are most commonly post-traumatic - accounting for 90% of all cases [4]. A CSF leak complicates a skull base fracture in 1-3% of closed head injuries [4]. About 80% of cases manifest with rhinorrhea and 20% with otorrhea [4]. Eighty percent of post-traumatic CSF leaks occur within the first 48 hours after injury, and 95% will manifest within the first 3 months [4]. Most traumatic leaks (up to 2/3's in some reports) close spontaneously and otorrhea reportedly has a greater chance compared to rhinorrhea [4]. A persistent CSF leak places the patient at increased risk of meningitis (4-50% of cases) or less frequently, intracranial abscess or encephalitis [4]. The diagnosis of CSF leak can be confirmed by obtaining a sample (at least 0.5 mL) of the secretions and measuring the beta2-transferring activity ( a protein highly specific for human CSF) [4].
Planar imaging can be performed following the intrathecal administration of either Tc-99m-DTPA or In-111-DTPA [4]. Patient positioning maneuvers (Trendelenburg) are performed to facilitate craniad flow of the tracer [4]. It is often also useful to have the patient in the position which is associated with the greatest leakage during this time (images should also be acquired in this position). Planar images are acquired at 2-4 hours and 24 hours following tracer administration in the anterior, posterior, and lateral projections [4]. More delayed imaging can be obtained (out to 72 hours) when using In-111-DTPA [4]. Radiotracer accumulation within the nasal cavity or nasopharynx confirms a leak [4]. One to two hours prior to the start of the examination, pledgets are placed by ENT or Neurosurgery in the anterior and posterior portion of each nasal region. The pledgets are left in for 24 hours after tracer administration [4]. Children may not tolerate the packs for more than a few hours and they can be placed 30 minutes after injection and removed after 4 to 6 hours if necessary. Counts are collected in a well counter and compared to counts from a plasma sample. A ratio of pledget to plasma radioactivity greater than 1.5-3.0:1 is considered positive for a leak [4]. Unfortunately, precise localization of the site of the leak may still be difficult as nasal secretions mix to collect on all of the pledgets on a given side [4].
CT findings suggestive of a CSF leak include a skull base bone defect and an air-fluid level or opacification of the contiguous sinus [4]. For the temporal bone, a unilateral opacified mastoid and middle ear, in the presence of a tegmen defect or fracture through an inner ear structure is consistent with a CSF fistula [4]. CT cisternography or MR imaging can also be performed to evaluate CSF leaks [4].
REFERENCES:
(1) J Nucl Med 1996; Vernet O, et al. Radionuclide shuntogram:
Adjunct
to manage
hydrocephalic patients. 37: 406-410
(2) J Nucl Med 1995; Shih W, et al, Reversible hypoperfusion of the cerebral cortex in noral-pressure hydrocephalus on technetium-99m-HMPAO brain SPECT images after shunt operation. 36: 470-473
(3) J Nucl Med 2003; Mataro M, et al. Postsurgical cerebral perfusion changes in idiopathic normal pressure hydrocephalus: a statistical parametric mapping study of SPECT images. 44: 1884-1889
(4) Radiology 2008; Lloyd KM, et al. Imaging of skull base cerebrospinal fluid leaks in adults. 248: 725-736
(5) AJR 2009; Chung JJ, et al. Intraabdominal complications
secondary to ventriculoperitoneal shunts: CT findings and review
of the
literature. 193: 1311-1317
(6) Radiographics 2013; Uliel L, et al. Nuclear medicine in the
acute
clinical setting: indications, imaging findings, and potential
pitfalls. 33: 375-396
(7) AJR 2020; Khalatbari H, Parisi MT. complications of CSF
shunts in pediatrics: functional assessment with CSF shunt
scinitgraphy- performance and interpretation. 215: 1474-1489